Ataxia
Table of Contents
What is Ataxia?
Ataxia occurs when you have a problem with coordination, causing you to move in an unsure, uncomfortable, or even clumsy manner. It typically indicates a problem with your brain, hearing, or other nervous system components.
A collection of conditions or a disease’s symptoms might be referred to as ataxia. Ataxia is a very prevalent symptom. Ataxia is a very uncommon disorder that occurs only in conjunction with specific hereditary abnormalities and illnesses.
What are the three major forms of ataxia?
There are three forms of ataxia, which manifest in various ways.
- Cerebellar ataxia is caused by a problem with the cerebellum, a portion of the brain that regulates how different areas of the brain interact.
- Sensory: Your body includes a “self-positioning” sense that allows your brain to monitor where each body component is. For example, you know where your hands and feet are even when you can’t see them. Sensory ataxia impairs your ability to perceive your position.
- Vestibular: This kind of involves an issue with your inner ears, which contribute to your sense of balance. With your sense of balance broken, it’s difficult to coordinate your movements.
What is Cerebellar Ataxia Syndrome?
The phrase cerebellar ataxia syndrome refers to a collection of symptoms rather than a single diagnosis or condition. Ataxia is defined as an unsteady walk or a lack of muscular coordination. Cerebellar refers to the brain’s cerebellum. The cerebellum is situated just above the spinal cord at the back and base of the skull. It processes information from other parts of the brain, the spinal cord, and sensory receptors. Its responsibilities include coordination and balance.
People with cerebellar ataxia syndrome may have an uneven walk or a loss of coordination due to cerebellar dysfunction. Cerebellar ataxia is characterized as acute (happens suddenly and swiftly) or chronic (happens gradually over time). It can also be recurring (occurs on and off over time) or progressive (deteriorates with time).
Cerebellar ataxia syndrome symptoms can arise with no clear explanation, but it can also be caused by a variety of illnesses, syndromes, and situations. Infectious disorders, hereditary or genetic problems, specific drugs, malignancies, trauma, and vascular issues are among examples. Because cerebellar ataxia syndrome can be caused by a variety of diseases, disorders, or conditions, it is critical to get an accurate diagnosis. If you experience an uneven stride, trouble walking or talking, or coordination issues, schedule a physical checkup with your doctor.
The actual incidence of cerebellar ataxia syndrome in the United States is unknown. However, it can occur at any age, in both men and women. Children under the age of three are more prone to develop acute cerebellar ataxia, which typically occurs after a viral illness, such as chickenpox. Adults are more prone to develop persistent cerebellar ataxia when combined with other neurological illnesses, such as multiple sclerosis or tumors.
Cerebellar ataxia syndrome is treated based on the underlying illness, ailment, or condition. Acute cerebellar ataxia induced by viral infections generally resolves without therapy after a few weeks. Treating other underlying illnesses, syndromes, or conditions can assist in alleviating symptoms. Otherwise, therapy is supportive and aims to alleviate symptoms and aid in everyday tasks.
Related Anatomy
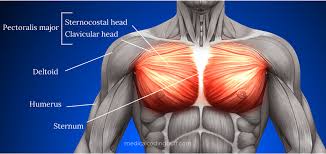
There are about 206 bones in the human body, and several ligaments connect them. About 650 skeletal muscles are supported by them, which makes movement easier. While the somatic nervous system primarily controls these skeletal muscles, involuntary impulses aid in the regulation of muscular tone, balance, and posture.
The cerebellum generates and regulates these impulses. In addition to the aforementioned functions, the cerebellum is in charge of coordinating volitional behaviors such as gymnastics done while racing to get dressed at 7:59 a.m. for an 8:00 a.m. anatomy class.
Origin and Location
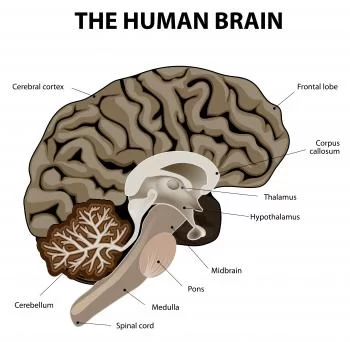
The cerebellum develops from the rhombencephalon or hindbrain. It is caused by the metencephalon’s rhombic lips or alar plates (dorsal thickening of the neural tube that produces the sensory regions of the nervous system), which span between the pontine flexure and the rhombencephalic isthmus.
It is an oval-shaped structure situated underneath the tentorium cerebelli in the posterior cerebral fossa. It has a grey matter cortex on the outside and white matter within.
Surfaces
The superior vermis, a centrally located, vertically projecting structure that runs anteroposteriorly, is visible on the superior (tentorial) surface of the cerebellum. The superior vermis begins at the front cerebellar notch and then curves 180 degrees to the posterior cerebellar notch. The inferior vermis runs along the center of the inferior (occipital) surface. The cerebellar hemispheres are located on the superior and inferior sides of the vermis.
Fissures
The cerebellum has many horizontal grooves on both surfaces, giving it a layered look. Some are more pronounced than others, providing appropriate demarcations for the lobes and lobules. One such groove is the horizontal fissure, which runs along the cerebellum’s lateral and posterior edges until it meets the posterolateral fissure (inferior to the flocculonodular lobe).
The postlunate fissure extends from left to right over the tentorial cerebellar surface. This is located posterior to the principal fissure that separates the anterior and posterior lobes. The major and postlunate fissures continue down the cerebellum’s inferior surface. Lastly, each cerebellar tonsil has a peritonsillar fissure running behind it.
Lobes
There are three primary lobes, nine lobules along the vermis, and five hemispheric lobules. The anterior lobe extends anteriorly from the cerebellar peduncles, including the anterior two-thirds of the superior vermis as well as the anterior third of each hemisphere. This lobe ends at the major fissure.
Up until it reaches the posterolateral fissure, the expanded posterior lobe crosses the inferior surface posteriorly and laterally. The flocculonodular lobe is the smallest. It is a flattened lobe situated between the superior cerebellar peduncles and the inferior medullary velum (superiorly) and the posterolateral fissure (inferior).
Cerebellar Peduncles
Three-foot processes bind the cerebellum to the brainstem while providing a channel for neuronal tracts to and from the cerebellum. These structures are known as the superior, middle, and inferior cerebellar peduncles. The connections between the cerebellum and the corresponding sections of the brainstem are as follows:
- To midbrain: superior cerebellar peduncles.
- To pons: middle cerebellar peduncles.
- To medulla: inferior cerebellar peduncles.
Blood Supply
The vertebrobasilar system originates in the first segment of the subclavian arteries and travels cranially through the transverse foramina of the upper six cervical vertebrae. The left and right vertebral arteries join at the pontomedullary junction, where they reach the cranial vault via the foramen magnum. It connects to form the basilar artery.
The cerebellum receives circulatory supplies from three main branches: two from the basilar component and one from each vertebral branch.
- The superior cerebellar artery is the basilar artery’s first branching point. It emerges bilaterally, inferior to CN III. It supplies circulation to the superior cerebellar region, as well as the superior medullary velum, pineal gland, and pons.
- The anterior inferior cerebellar artery (AICA) emerges inferior to CN VI at the pontomedullary junction, near the proximal section of the basilar artery. It subsequently shifts posterolaterally to service the inferior and anterior cerebellar regions.
- Third, a posterior inferior cerebellar artery (PICA) emerges from each vertebral artery immediately above the rootlet of CN XI. It delivers arterial blood to the cerebellar nucleus and inferior surface (including the vermis).
Causes of Ataxia
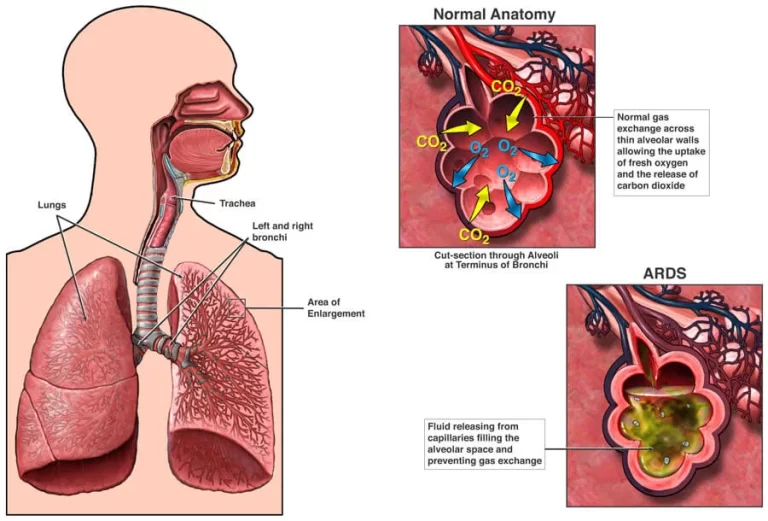
Ataxia is caused by injury to the cerebellum and its connections. The brainstem is connected to the cerebellum, which is situated close to the base of the brain. The cerebellum regulates balance, eye movement, swallowing, and speech.
There are three main types of ataxia causes: acquired, degenerative, and inherited.
Acquired causes
- Alcohol: Long-term excessive alcohol use may result in persistent ataxia. Ataxia can be improved by abstaining from alcohol.
- Medicines: Ataxia is a possible adverse effect of some medications. Sedatives like benzodiazepines and phenobarbital can cause it. It may also be caused by anti-seizure medications, particularly phenytoin. Some chemotherapy treatments may also cause ataxia.
- Toxins: Heavy metal toxicity, such as lead or mercury, as well as solvent intoxication, such as paint thinner, can also produce ataxia.
- Certain vitamins are either insufficient or overabundant: Ataxia can be caused by insufficient vitamin E, vitamin B-12, or vitamin B-1, often known as thiamine. Ataxia can also result from a
- Lack or excess of vitamin B-6: A vitamin deficit occurs when there is insufficient intake of a
- Specific vitamin: When a vitamin shortage is the cause of ataxia, it is generally treatable.
- Thyroid conditions. Both hypothyroidism and hypoparathyroidism can produce ataxia.
- Stroke: A stroke causes sudden onset of ataxia. This could be caused by a blood vessel obstruction or bleeding in the brain.
- Multiple Sclerosis: This disease can produce ataxia.
- Autoimmune disorders: Ataxia can be caused by a variety of autoimmune illnesses, which occur when the immune system destroys healthy cells. Sarcoidosis is a disease that causes
- Inflammatory cells cluster in certain regions of the body: They may also include celiac disease, which is caused by an immunological sensitivity to gluten. Ataxia can also be induced by encephalomyelitis, a disorder characterized by swelling in the brain and spinal cord.
- Infections: Ataxia in children can occasionally be a symptom of chickenpox, as well as other viral infections such as HIV and Lyme disease. It may arise during the healing stages of the infection and last for several days or weeks. The symptom normally improves with time.
- COVID-19: Ataxia can be caused by a severe infection with the COVID-19 virus.
- Paraneoplastic syndromes: These are rare degenerative disorders caused by the immune system’s response to a malignant tumor, known as a neoplasm. The most common causes of paraneoplastic syndromes are lung, ovarian, or breast cancer, as well as lymphomas. Ataxia might appear months or years before the tumor is diagnosed.
- Changes to the brain: An infected region in the brain, known as an abscess, can induce ataxia. A brain tumor, whether malignant or noncancerous, can cause damage to the cerebellum.
- Head trauma: Ataxia can result from brain injury.
- Cerebral palsy: This word refers to a range of disorders induced by brain injury in children. The injury may occur before, during, or shortly after birth. It impairs the child’s capacity to coordinate physical motions.
Degenerative causes
Multiple system atrophy. This rare condition affects blood pressure and other movements and processes. It can induce ataxia and other symptoms such as loss of bladder control, fainting after standing up, and a sleep behavior disorder in which a person plays out nightmares.
Hereditary causes
Certain kinds of ataxia and the variables that cause them are handed down through generations. These conditions are also referred to as hereditary diseases. If you have one of these diseases, you may have been born with a genetic mutation that causes your body to manufacture unusual proteins.
The abnormal proteins interfere with nerve cell function, particularly in the cerebellum and spinal cord. They cause degeneration, or the breakdown and death of nerve cells. As the condition advances, coordination issues deteriorate.
People with genetic ataxia may have acquired a dominant gene from one parent, resulting in an autosomal dominant inheritance pattern. Alternatively, they may have acquired a recessive gene from both parents, resulting in an autosomal recessive inheritance pattern. A recessive condition does not impact the parents, but it may affect siblings.
Different gene alterations result in different forms of ataxia. Most types worsen over time. Each type produces poor coordination but also exhibits other distinct symptoms.
Autosomal dominant ataxias
Spinocerebellar ataxias: More than 40 genes for spinocerebellar ataxia have been found by researchers, and the list is growing. All forms share ataxia and cerebellar degeneration, however there may be additional symptoms.
Episodic ataxia (EA): There are eight known kinds of episodic ataxia. The most prevalent varieties are EA1 and EA2. EA1 causes transient bouts of ataxia that can last seconds or minutes. Stress, unexpected movement, or being startled can all cause episodes. They are frequently linked with muscle twitching.
EA2 causes lengthier spells of ataxia, ranging from 30 minutes to six hours. These episodes are also provoked by stress. You may have dizziness and muscle weakness. People with EA2 may feel extremely weary. Sometimes symptoms improve later in life. Episodic ataxia does not shorten life, and the symptoms may respond to medication.
Autosomal recessive ataxias
Friedreich’s ataxia: This is the most prevalent inherited ataxia. It causes damage to the cerebellum, spinal cord, and peripheral nerves. Peripheral nerves carry impulses from the arms and legs to the brain and spine. Symptoms often begin before age 25. A brain scan normally does not reveal alterations in the cerebellum with this kind of ataxia.
The first symptom of Friedreich ataxia is usually difficulty walking. Frequently, as the disease worsens, the arms and trunk are affected. This type of ataxia can produce alterations in the feet, such as elevated arches. It can also induce a spinal curvature known as scoliosis.
Other symptoms that may occur include slurred speech, weariness, abnormal eye movements, and hearing loss. Friedreich ataxia can also cause cardiac enlargement, which is known as cardiomyopathy. Diabetes and heart failure are both possible outcomes. Early treatment for heart problems can enhance both quality of life and survival.
RFC1-associated ataxia: This is the most common cause of ataxia that manifests later in life. Symptoms of ataxia typically include dizziness, numbness, or tingling throughout the body. This sort of ataxia might induce a cough.
Ataxia-telangiectasia: This rare pediatric condition degenerates the brain and immune system. This increases the likelihood of developing additional disorders, such as infections and cancers.
Telangiectasia is the growth of small red “spider” veins in the corners of a child’s eyes, as well as on their ears and cheeks. Delayed motor skill development, poor balance, and slurred speech are frequently the initial symptoms. Frequent sinus and respiratory infections are prevalent.
Children with ataxia-telangiectasia have an increased chance of acquiring cancer, particularly leukemia or lymphoma.
Congenital cerebellar ataxia: This kind of ataxia is caused by birth-related cerebellar injury.
Wilson’s Disease: People with this illness accumulate copper in their brains, liver, and other organs. This can result in ataxia, among other symptoms.
Signs and Symptoms
Initial ataxia symptoms typically include:
- Poor limb coordination.
- Dysarthria refers to slurred and sluggish speech that is difficult to produce. Pitch, rhythm, and volume control issues may also be present in the patient.
- As the ataxia advances, more symptoms may appear: Swallowing issues can sometimes cause choking or coughing.
- Facial expressions become less noticeable.
- Tremors: Inadvertent shaking or trembling of bodily parts is possible.
- Nystagmus is an involuntary, fast, rhythmic, and repetitive eye movement.
- Movements might be vertical, horizontal, or circular.
- Cold feet occur due to a lack of muscle activation.
- Problems with balance.
- Walking difficulties: In severe circumstances, the patient may require a wheelchair.
- Vision issues.
- Hearing difficulties.
- Depression – as a result of having to live and deal with the symptoms.
Types of Ataxia and their characteristics
Injuries to different motor or sensory components of the central nervous system as well as diseases of the peripheral nerves can result in ataxia (Bastian 1997). Ataxia can be caused by problems with the cerebellum, proprioceptive system, visual system, vestibular system, or any of their connections.
Some researchers (Bastian 1997) divide ataxia into two types, whilst others (Morgan 1980) divide it into three categories: vestibular, cerebellar, and sensory ataxia. According to Erasmus (2004), some authors categorize frontal ataxia into a fourth group. Mixed ataxia refers to a scenario in which symptoms from two or three different ataxia categories are present (Edwards 1996).
Sensory ataxia:
Because the dorsal columns of the spinal cord send proprioceptive information to the brain, ataxia caused by loss of proprioception—or sensitivity to joint and body part position—is known as sensory ataxia. The thalamus and parietal lobes, among other brain regions that receive that information, may malfunction under specific circumstances. When proprioceptive input is absent and cannot be supplied by visual input, sensory ataxia manifests as an unsteady “stomping” walk with heavy heel strikes and postural instability.
When a patient stands with their feet together and their eyes closed, their stability deteriorates, potentially leading to massive oscillations and a collapse. The most crucial finding distinguishing sensory ataxia from other types of ataxia is that it results in a positive Romberg test (Bannister 1992). Sensory ataxia is distinguished by the lack of deep tendon reflexes and vibration awareness in the extremities. Another symptom of sensory ataxia is a deterioration of the finger-pointing test with the eyes closed.
Hereditary ataxias, such as Friedreich’s ataxia and spinocerebellar ataxia, can cause sensory ataxia. Sensory ataxia can also be caused by illnesses such as vitamin B12 deficiency neuropathy, diabetic or alcoholic neuropathy, tabes dorsalis, tumors in the posterior cord of the medulla spinalis, and multiple sclerosis.
Vestibular ataxia:
Diseases of the peripheral or central nervous systems that directly affect the vestibular nuclei or their afferent and efferent connections can induce vestibular ataxia. A patient with vestibular ataxia has difficulty maintaining balance whether sitting or standing. The patient has a broad base of support, staggers when walking, and occasionally leans to one side or the other. Head and trunk movements commonly cause arm mobility to be restricted.
The patient is limited because it is difficult for him or her to keep balance when making head or eye movements, particularly when crossing the street or shopping at the market. Vestibular ataxia can be accompanied by vertigo, nausea, vomiting, blurred vision, and nystagmus due to the vestibular system’s function in detecting and experiencing self-motion and stabilizing gaze via the vestibular-ocular reflex (Horak & Shupert 1994). Extremity ataxia is not a feature of vestibular ataxia. Deep tendon reflexes are thought to be typical.
Vestibular ataxia can be caused by both central (multiple sclerosis and medullary stroke) and peripheral vestibular illnesses (Menier’s, hydrops, benign paroxysmal vertigo, or vestibular neuronitis).
Cerebellar ataxia:
Cerebellar ataxia can arise as a result of a cerebellar lesion or damage to its afferent and efferent pathways.
Vestibulo-cerebellar dysfunction affects balance regulation and eye movement control and is linked to the flocculonodular lobe (flocculus and modulus). Postural instability is characterized by a tendency to separate feet when standing to create a wider base and prevent oscillations, particularly posterior-anterior ones; standing with feet together exacerbates instability regardless of whether the eyes are open or closed, as evidenced by a negative Romberg’s test (en.wikipedia.org, Liao et al. 2008, Morton&Bastian 2004).
Spinocerebellar dysfunction, which affects the vermis and paravermis, results in a wide-based gait with abnormal patterns of inter-joint coordination, lateral deviations, uneven steps, and unpredictable start and stop. Walking incoordination, sometimes referred to as gait ataxia, is a result of injuries to this area of the cerebellum.
Dysfunction of the cerebral-cerebellum relationship indicates a lesion in the deep pontine nuclei. Damage to the cerebrocerebellum, which is responsible for movement planning and monitoring, reduces the ability to perform voluntary, planned movements (Chmahmann 2004).
Risk factors
There are several risk factors for ataxia. People with a family history of ataxia have an increased risk of developing it themselves.
Other risk factors are:
- Long-term excessive alcohol consumption.
- Have hypothyroidism or hypoparathyroidism.
- I have multiple sclerosis.
- Celiac disease is a condition caused by an immunological reaction to gluten.
- A condition called sarcoidosis causes an accumulation of inflammatory cells throughout the body.
- Multiple system atrophy is a degenerative condition.
- A paraneoplastic condition caused by cancer.
- Taking anti-seizure medications and sedatives increases the risk of ataxia.
- Being exposed to heavy metals such as lead or mercury, as well as solvents like paint thinner.
Diagnosis
Your healthcare practitioner searches for a treatable reason when diagnosing ataxia. You will most likely have physical and neurological examinations. Your healthcare expert will assess your eyesight, balance, coordination, and reflexes. You might also need:
- Blood testing: These may assist in identifying treatable causes of ataxia.
- Image studies: An MRI of the brain could assist in determining the various causes. Sometimes, in ataxia sufferers, an MRI will show shrinkage of the cerebellum and other brain regions. It may also reveal other curable conditions, such as a blood clot or a benign tumor.
- Spinal tap, often called lumbar puncture: This test may be useful if an infection, swelling (also known as inflammation), or certain disorders are producing ataxia. An implanted needle is used to extract a small amount of cerebrospinal fluid from between two lower back bones. The fluid that surrounds and protects the brain and spinal cord is transported to a lab for analysis.
- Genetic testing: To ascertain whether a gene alteration is responsible for an ataxia-related ailment, your doctor could recommend genetic testing. Many inherited ataxias can be diagnosed using gene tests, but not all.
Treatment of Ataxia
Ataxia treatment is determined by the underlying cause. If ataxia is caused by a condition like vitamin insufficiency or celiac disease, addressing it can help alleviate symptoms. If ataxia is caused by chickenpox or another viral infection, it will most likely resolve on its own.
Friedreich ataxia can be treated with an oral medication known as omaveloxolone (Skyclarys). The drug was approved by the United States Food and Drug Administration for adults and teenagers aged 16 and up. In clinical trials, taking the medication alleviated symptoms. Omaveloxolone can influence liver enzyme and cholesterol levels, thus people who use this medication should have regular blood tests. Omaveloxolone’s potential adverse effects include headache, nausea, stomach pain, lethargy, diarrhea, and muscular and joint pain.
Other medications may alleviate symptoms like stiffness, tremors, and disorientation. Your healthcare practitioner may also prescribe adapting gadgets or therapies.
Adaptive devices
Multiple sclerosis and cerebral palsy can also cause ataxia, which may not be curable. However, adaptive gadgets may assist. They include:
- For walking, use hiking sticks or walkers
- Modified eating utensils
- Communication tools for speaking
Therapies
You may benefit from specific therapies, including:
- PT can help with mobility and coordination improvement.
- Occupational therapy to help with everyday tasks like self-feeding.
- Speech therapy facilitates swallowing and enhances speech.
- Studies have indicated that certain ataxia sufferers may benefit from strength and aerobic exercise.
Physiotherapy Treatment and Rehabilitation of Ataxia
- The physiotherapist’s goal in the rehabilitation of ataxia caused by deficiencies in neurological structures that impair the patient’s functions is to enhance the patient’s functional level using restorative approaches.
- When this is not possible, the therapist employs compensatory measures to help the patient function as independently as possible within their current functional level.
- Restorative physical therapy aims to improve balance and posture in response to external stimuli and gravity.
- Improving and expanding postural stabilization after the establishment of joint stabilization.
- Developing upper extremity functions.
- Developing an independent and functional gait improves the patient’s quality of life by enhancing independence while conducting everyday activities.
Main principles of training
- Exercises should be performed consciously at the beginning of the training program and then automatically as it progresses.
- The activities ought to advance from easy to difficult.
- Practice exercises with your eyes open at first, then with them closed.
- Once proximal tonus and stability have been achieved, assess how well the distal portions move together.
- When necessary, supportive aids and equipment should be used in addition to compensation measures.
- Sports and an appropriate at-home exercise program should be combined with treatment.
Measurement and assessment
- To achieve the desired goal of the physiotherapy and rehabilitation program in the treatment of ataxia, it is critical to identify treatment programs that are appropriate for the patient and his or her needs.
- This can be accomplished by employing suitable measuring and assessment techniques, as well as interpreting the results.
- In addition to creating an appropriate treatment plan, measurement and evaluation are used to track a patient’s progress over time and track the results of the treatment.
- Ataxia circumstances are made worse by standardization problems in evaluation and measurement, which are among the most upsetting aspects of neurological rehabilitation applications.
- More scales, observational techniques, and computer systems developed to measure balance and in-coordination are found in the literature.
- While scales and observational methods primarily intended for balance assessment are easy to use and practical in the clinic, their ability to provide consistent data is limited, and the outcomes may vary based on the observer.
- Despite their excellent reliability, computerized systems are costly and require a laboratory environment to operate. Physiotherapists regularly use balance evaluation instruments.
Methods of balance assessment
External Perturbation Test(Push and Release Test):
- External Perturbation Test – Pull test: Static balance’s objective in different sensory contexts.
- The Clinical Sensory Integration Test is designed to evaluate dynamic balance in a variety of sensory situations.
- Sensory Integration Test of Computerized Dynamic Posturography:
- The aim is static and dynamic equilibrium.
- Single Leg Stance Test: The purpose of static equilibrium.
Functional Reach Test:
What is the aim of functional static and dynamic balance?
- The aim of the five-times sit-to-stand test is to examine functional dynamic balance and gait.
- Time Up and Go Test: assess Gait and Functional Dynamic Balance.
- The aim of dynamic balance and gait is assessed by the Dynamic Gait Index.
- Tandem walking helps the aim of maintaining dynamic equilibrium.
- The Four Square Step Test helps assess dynamic balance.
- In addition to these tests, gait duration, step length, and step breadth can be measured. Patients can assist with assessment methods by using self-perception scales such as the Dizziness Handicap Inventory, Activity Specific Balance Confident Scale, and daily living scales like the Barthel Index and FIMTM.
- There are very few scales that have been developed and evaluated for validity and reliability in order to evaluate both extremity ataxia and truncal ataxia.
Scales of ataxia
- Speech, nystagmus, gait ataxia, and truncal and extremity ataxia are all evaluated using the International Cooperative Ataxia Rating Scale.
- Speech, gait, and truncal and extremity ataxia are all assessed using the Scale for Assessment and Rating of Ataxia.
- The Ataxia Functional Composite Scale evaluates gait speed, upper extremity ataxia, and visual acuity.
- One examination test for upper limb ataxia is the Nine Hole Peg Test.
- Upper limb ataxia assessed using a computer graphics tablet.
- The Short Ataxia Rating Scale evaluates speech, nystagmus, gait ataxia, and truncal and extremity ataxia.
- Friedreich’s ataxia impact scale includes speech, upper and lower limb function, body movement, difficult tasks, isolation, mood, and self-perceptions.
- Upper limb functions contribute to the composite cerebellar functional severity score.
Physiotherapy approaches
- A physical therapy plan is developed by interpreting the measurement and evaluation data.
- The components of the treatment regimen may differ based on the type and characteristics of the ataxia.
- Stability training is more crucial in lowering truncal and extremity ataxia in patients with cerebellar ataxia, even if therapies that enhance proprioception and include visual aids are more frequently used in patients with sensory ataxia.
- Patients with vestibular ataxia should be given habituation exercises to reduce vertigo, as well as vestibulo-ocular and vestibulo-spinal reflex stimulation to improve balance.
- Mixed ataxia is one example of a challenging condition that necessitates the employment of many approaches.
- In such circumstances, the physiotherapist’s experience and the patient’s effort are key factors in defining the program.
- When developing the therapy prescription, keep in mind that the proprioceptive, vestibular, and visual systems, as well as the cerebellum, are all interconnected and that this relationship results in balance and coordination.
- Proprioceptive exercises, for example, improve both balance and proprioception. The contrary is also true. Approaches to treating extremities ataxia may allow for increased proprioceptive input and the development of balance via stabilizing.
- As a result, the treatments used in ataxia rehabilitation cannot be classified as approaches focused solely on proprioception or balance, because they all interact with one another.
The classification of therapy applications can be summarized as follows:
Approaches to improve proprioception:
- The goal is to increase proprioceptive input by manually stimulating joint surfaces, muscles, and tendons while minimizing postural instability through improved body awareness.
- Numerous ways can be taken for this objective. These include proprioceptive neuromuscular facilitation (PNF), rhythmic stabilization, slow reversal techniques, resistive exercises, the use of Johnstone pressure splints, gait exercises on various surfaces (hard, soft, inclined) with eyes open and closed, plyometric exercises, balance board ball, and minitrampoline exercises.
- Recently, vibration has become a popular use. Vibration can be delivered directly to muscles and tendons or the entire body.
- Appropriate treatment is an additional choice. The suit is made up of knee pads, a vest, shorts, and unique shoes that are fastened with bungee-style bands. Its purpose is to provide resistance and help the wearer position their body correctly while doing movements.
- Its primary goals are to improve proprioception (feeling from joints, fibers, and muscles) and to promote weight-bearing for normalized sensory input during posture and movement.
- Furthermore, approaches that promote body awareness, such as the Feldenkrais and Alexandre Techniques, yoga, and body awareness exercises, can be incorporated into the program.
Exercises to Improve Balance
- First, the proximal muscles and trunk stability should be addressed. The PNF techniques’ mat activities are suited for this purpose.
- Following the neuro-developmental order, the patient should be trained to come to the bridge position from lying on the back, onto the forearms from lying face down, crawl, and come onto the knees, half knees, and into a sitting position, as well as to establish static and dynamic stability in these positions.
- Initially, the patient should be kept in the proper position using approximation and verbal instructions, and subsequently, static stability should be strengthened by external perturbation (pushing and pulling in different directions).
- The patient should next be trained in these positions for weight transfer and functional extension to prepare for dynamic stabilization.
- Subsequently, the patient should be taught in positions where the support surface is reduced or the center of gravity is altered to make balance exercises more challenging. (For example, creating balance on two or three limbs while crawling or changing the center of gravity upward by elevating the arms while sitting on the knees).
- Balance training on one leg should be performed in the standing position after transferring weight to the front, back, and sides, narrowing the support surface, and tandem position. Ataxic patients benefit greatly from this stance.
- Another approach is to use the posturography device for balance training to gain visual feedback from observing the patient’s ability to maintain postural oscillation in the center of gravity.
- Gait is the strongest measure of dynamic stability and balance. As a result, gait training should include the following exercises: walking in two narrow lines, tandem gait, backward gait, slower gait (soldier’s gait), pausing and turning in reaction to sudden directions, flexion, extension, and left-right head rotations.
- Tai Chi and Yoga are two disciplines that focus on developing balance.
Vestibular exercises:
- Because dizziness is associated with balance impairment in vestibular issues, repetitive head motions as well as Cawthorne and Cooksey exercises are quite important.
- A vestibular training program consists of repetitive, increasingly challenging eye, head, and body movements intended to promote movement and sensory substitution. Physical and occupational therapists still employ many of the components of this workout regimen
Approaches to extremity ataxia:
- Exercises meant to cure limb ataxia give fixation by establishing a balance between eccentric and concentric contractions within the multi-joint movements of the lower and upper extremities, respectively.
- These exercises require slow, controlled, and reciprocal multi-joint movement and stabilization. Frenkel’s coordination exercises were designed for this aim. Actively repeated contractions, comparable to PNF, can be used alone or in combination with Freenkel’s coordination exercises.
- While these two types of exercise are useful for mild extremities ataxia, they may be insufficient in more severe cases. In such circumstances, rhythmic stability and a mix of isotonic approaches are superior to PNF.
- Dr. Giselher Schalow created Coordination Dynamics Therapy (CDT). He claims that this treatment “Improves the self-organization of the neuronal networks of the CNS for functional repair by exercising extremely exact coordinated arm and leg movements on a special device (GIGER MD).
Use of supportive aids:
In circumstances where restorative physical therapy applications are insufficient, the use of supportive devices allows the patient to perform more comfortably within his current functional level. In cases of severe ataxia, suspending weights from the extremities and using weighted walkers may be preferable.
Sports activities:
Horseback riding, swimming, billiards, golf, and darts are all appropriate activities for this patient.
Counseling:
Patients with ataxia frequently become irritated and depressed as a result of dealing with symptoms that impair physical mobility and coordination. Talking with a trained counselor, such as a psychotherapist, can assist.
Supplements and nutrition:
Some people with ataxia have extremely low vitamin E levels, necessitating supplementation and/or a particular diet. A gluten-free diet may be beneficial for certain people with ataxia because they are sensitive to gluten.
Medication:
Some people with ataxia telangiectasia are given gamma-globulin injections to enhance their immune systems. There are other medications for muscular spasms and uncontrolled eye movements.
Summary
Cerebellar ataxia is a neurological disorder characterized by impaired coordination and balance, primarily resulting from damage or dysfunction of the cerebellum. The cerebellum, located at the base of the brain, plays a crucial role in motor control, coordination, and fine-tuning of movement. When this area is affected, it leads to a range of symptoms that significantly impact a person’s ability to perform everyday tasks.
The symptoms of cerebellar ataxia typically include unsteady gait, poor balance, difficulty with fine motor tasks, slurred speech, and abnormal eye movements. Patients may also experience tremors, particularly when trying to perform specific actions. The severity of symptoms can vary widely among individuals and may worsen over time, depending on the underlying cause.
Cerebellar ataxia can be caused by various factors, including genetic mutations, stroke, tumors, infections, toxins, and certain medications. In some cases, it may be part of a broader neurological condition. Diagnosis often involves a combination of neurological examinations, imaging studies such as MRI, and genetic testing when a hereditary form is suspected.
Treatment for cerebellar ataxia is primarily focused on managing symptoms and addressing the underlying cause when possible. This may include physical therapy to improve balance and coordination, occupational therapy to assist with daily living activities, and speech therapy to address communication difficulties. In some cases, medications may be prescribed to alleviate specific symptoms or treat associated conditions.
Research into cerebellar ataxia is ongoing, with scientists exploring potential therapeutic approaches, including gene therapy for hereditary forms and neuroprotective strategies to prevent further cerebellar damage. While there is currently no cure for most forms of cerebellar ataxia, early diagnosis, and appropriate management can significantly improve the quality of life for affected individuals.
FAQs
What is cerebellar ataxia?
Cerebellar ataxia is a neurological disorder characterized by impaired coordination and balance due to damage or dysfunction of the cerebellum.
What are the main symptoms of cerebellar ataxia?
The main symptoms include unsteady gait, poor balance, difficulty with fine motor tasks, slurred speech, abnormal eye movements, and sometimes tremors.
What causes cerebellar ataxia?
Causes can include genetic mutations, stroke, tumors, infections, toxins, certain medications, and sometimes it’s part of a broader neurological condition.
Is cerebellar ataxia hereditary?
Some forms of cerebellar ataxia are hereditary and can be passed down through families, while others are acquired due to external factors.
How is cerebellar ataxia diagnosed?
Diagnosis typically involves neurological examinations, imaging studies like MRI, and sometimes genetic testing for hereditary forms.
Can cerebellar ataxia be cured?
There is currently no cure for most forms of cerebellar ataxia, but treatments can help manage symptoms and improve quality of life.
What treatments are available for cerebellar ataxia?
Treatments may include physical therapy, occupational therapy, speech therapy, and sometimes medications to manage specific symptoms.
Does cerebellar ataxia affect lifespan?
The impact on lifespan varies depending on the underlying cause and severity. Some forms progress slowly and have minimal impact, while others can be more severe.
Is there ongoing research for new treatments?
Yes, researchers are exploring various approaches, including gene therapy for hereditary forms and neuroprotective strategies to prevent further cerebellar damage.
References:
- Cerebellar ataxia. (2023, July 27). Kenhub. https://www.kenhub.com/en/library/anatomy/cerebellar-ataxia
- Professional, C. C. M. (n.d.-a). Ataxia. Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/17748-ataxia#care-and-treatment
- Cerebellum gross anatomy. (2023, October 30). Kenhub. https://www.kenhub.com/en/library/anatomy/cerebellum-gross-anatomy
- Dhameliya, N. (2022, April 6). Cerebellar Ataxia: Cause, Symptoms, Diagnosis, Treatment, Exercise. Mobility Physiotherapy Clinic. https://mobilephysiotherapyclinic.net/cerebellar-ataxia-physiotherapy-treatment/#Sign_and_Symptoms
- Delgado, A. (2024, January 9). Acute Cerebellar Ataxia (ACA). Healthline. https://www.healthline.com/health/acute-cerebellar-ataxia#in-adults
- Physiotherapist, N. P. (2023a, November 24). Ataxia Cause, Signs and Symptoms, Diagnosis, Treatment. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/ataxia-physiotherapy-treatments-and-rehabilitation/#Signs_and_Symptoms_of_Ataxia
- Dhameliya, N. (2024, May 30). Cerebellar Ataxia: Cause, Symptom, Physiotherapy Treatment. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/cerebeller-ataxia/#Investigation
- Ataxia – Diagnosis and treatment – Mayo Clinic. (2024, January 30). https://www.mayoclinic.org/diseases-conditions/ataxia/diagnosis-treatment/drc-20355655
- Images: https://www.natural-health-news.com/wp-content/uploads/2015/05/Ataxia.jpg