Abstract and Introduction
Abstract
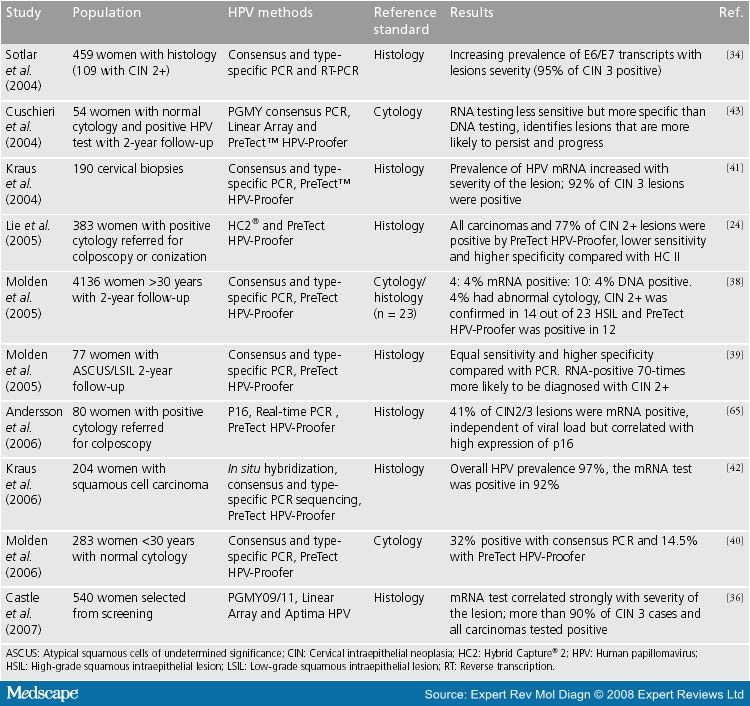
Human papillomavirus (HPV) is necessary for the development of cervical carcinoma, and incorporation of molecular testing for HPV in screening and patient management has been proposed. Sufficient scientific evidence exists to recommend HPV DNA testing in the triage of women with equivocal cytology and in follow-up after the treatment of precursor lesions. However, due to a low clinical specificity and positive predictive value, HPV DNA testing has so far not been recommended as primary screening in Europe. In general, diagnostic HPV tests have to demonstrate accuracy, reproducibility and clinical utility before they can be used in patient management and implemented in cervical cancer screening programmes. In this article we give an overview of RNA-based HPV diagnostics and the role of E6/E7 mRNA detection as a predictive marker for the development of cervical carcinoma. HPV E6/E7 mRNA testing for high-risk types seems to correlate better with the severity of the lesion compared with HPV DNA testing, and is a potential marker for the identification of women at risk of developing cervical carcinoma. Commercial assays for simultaneous genotyping and detection of E6/E7 mRNA from the five most common high-risk HPV types are now available and require further evaluation for primary screening, triage and follow-up after treatment.
Introduction
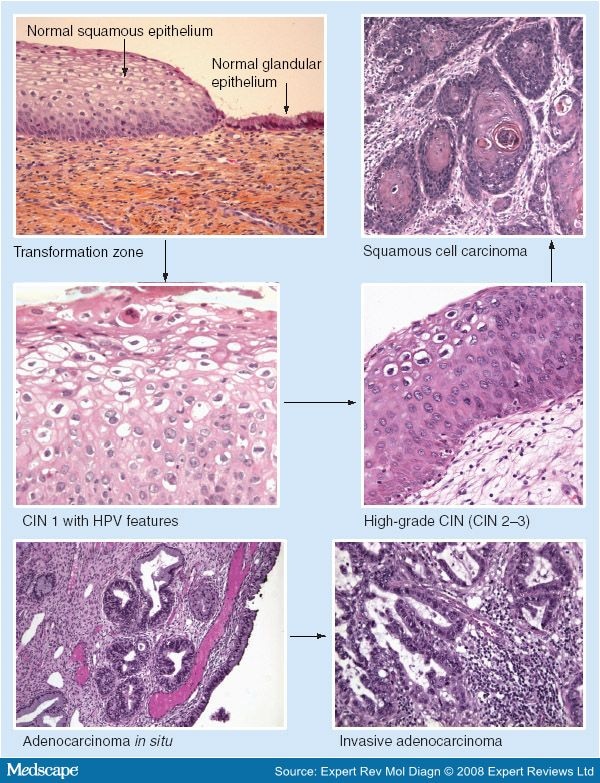
Cervical cancer is the second most common cancer among women worldwide with approximately 493,000 new cases and 274,000 deaths in 2002.[1] The majority of cases appear between the ages of 30 and 50 years when women are actively involved in their careers and caring for their families. Consequently, the total years-of-life lost is much higher than for other female cancers, which have a later age of onset. Some types of human papillomavirus (HPV) have been established as the central cause of cervical carcinoma.[2,3,4] Both premalignant and malignant epithelial lesions of the cervix are associated with HPV (Figure 1).
Persistent high-risk human papillomavirus infection may, over years, lead to precancerous lesions and invasive cervical carcinoma. Most cervical precancerous lesions and cervical carcinomas arise within the transformation zone (as shown in the top left-hand photo). HPV is thought to access the basal cells through microabrasion of the squamous epithelium. CIN: Cervical intraepithelial neoplasia; HPV: Human papillomavirus.
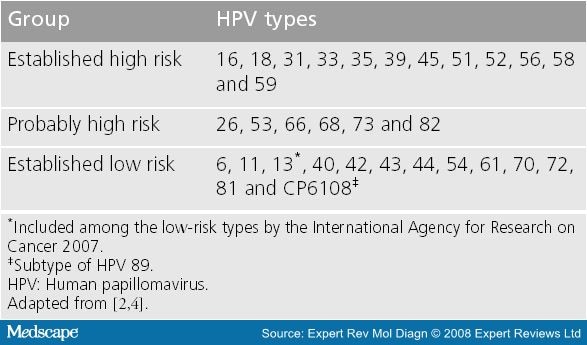
HPV is the most common sexually transmitted infection among men and women, and it has been estimated that 70% of sexually active women will acquire an HPV infection at some point during their lifetime.[5] More than 100 different genotypes have been isolated, and at least 40 infect the epithelial lining of the anogenital and aerodigestive tract.[6] Based upon epidemiologic studies, HPV viruses are classified as high-risk, probably high-risk and low-risk types ( Table 1 ).[7] Persistent infection with one of the high-risk types is the first step in carcinogenesis.[8] The vast majority of HPV infections are asymptomatic and transient, especially in the young population, and more than 90% of new infections will resolve within 2 years.[9] It is not clearly understood, however, why HPV infections resolve in certain individuals, but result in high-grade cervical neoplasia in others.[10] Several viral and host factors are thought to play a role in cervical carcinogenesis. Established cofactors are smoking, long-term oral contraceptive use, HIV co-infection and high parity, while HSV-2, Chlamydia trachomatis, immunosuppression, diet and nutrition are probable cofactors.[2] Worldwide, pooled data from case-control studies indicate that HPV DNA can be detected in 99.7% of women with histo ogically confirmed squamous cell carcinoma and in 13.4% of control women with normal cytology.[2]
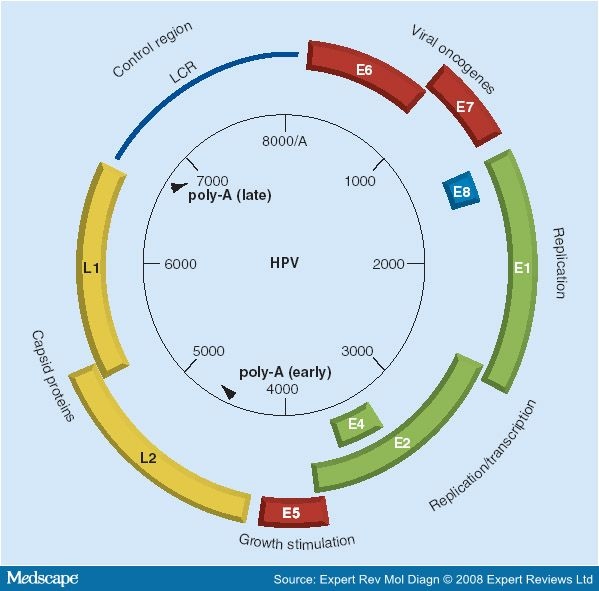
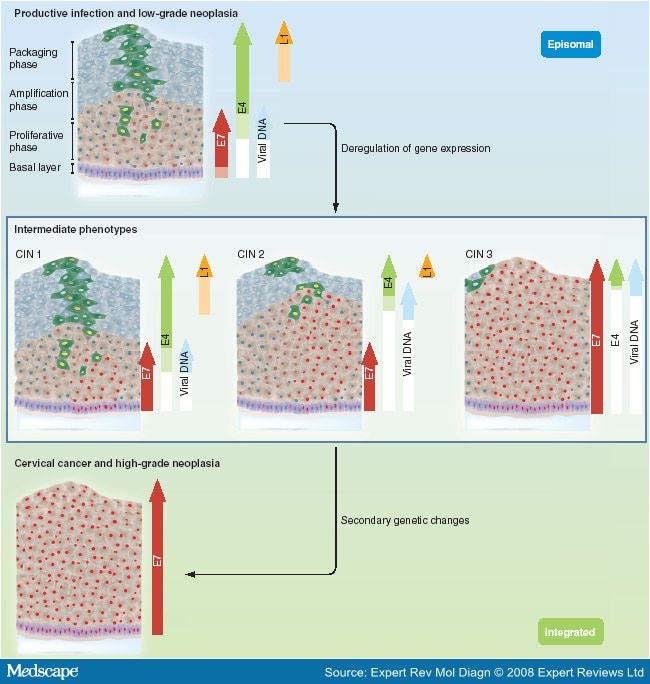
HPVs are small, non-enveloped DNA viruses, approximately 55 nm in diameter, that infect basal cells and replicate in the nucleus of squamous epithelial cells. The genomic organization of each of the papillomaviruses is remarkably similar and can be divided into three functional regions (Figure 2). Following infection, the early HPV genes (E6, E7, E1, E2, E4 and E5) are expressed and the viral DNA replicates from the episomal form of the virus. In the upper layer of the epithelium the viral genome is replicated further, and the late genes (L1 and L2) and E4 are expressed (Figure 3). The shed virus can then initiate new infections. Low-grade intraepithelial lesions support productive viral replication. Progression to high-grade intraepithelial lesions and invasive carcinomas is associated with a persistent high-risk HPV infection and integration of the HPV genome into the host chromosomes, loss or disruption of E2 and subsequent upregulation of E6 and E7 expression (Figure 3).[8,10,11] E6 and E7 are the oncogenes of the virus and expression of these genes is required for malignant transformation. Among others, E6 and E7 mediate degradation of the tumor suppressors p53 and RB, respectively, and interfere with cell-cycle regulation.[8,10] E6 and E7 proteins from low-risk types are less competent in interfering with p53 and pRb functions than E6/E7 proteins from high-risk types.[12,13] Therefore, low-risk HPV infections are associated with benign proliferations, such as genital warts and low-grade intraepithelial lesions prone to regress.
Genome organization of the papillomavirus. HPV16 from the α9 group of papillomaviruses. HPV: Human papillomavirus; LCR: Long control region. Reproduced with permission from Thomas Iftner.
Changes in viral gene expression accompanying the progression from cervical intraepithelial neoplasia to squamous cell carcinoma. Expression of E6/E7 oncogenes increases with the severity of the lesion. In cervical carcinoma the virus is integrated into the host cell chromosomes, this leads to further deregulation of E6/E7 expression. CIN: Cervical intraepithelial neoplasia. Reproduced with permission from Portland Press Limited.[11]
No writing assistance was utilized in the production of this manuscript.
Expert Rev Mol Diagn. 2008;8(4):405-415. © 2008 Expert Reviews Ltd.
Cite this: Human Papillomavirus E6/E7 mRNA Testing as a Predictive Marker for Cervical Carcinoma - Medscape - Jul 01, 2008.








Comments