LFT L - 4.pptx
- 1. Liver Function Tests (LFTs) Lecture - 4
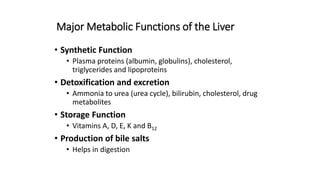
- 2. Major Metabolic Functions of the Liver • Synthetic Function • Plasma proteins (albumin, globulins), cholesterol, triglycerides and lipoproteins • Detoxification and excretion • Ammonia to urea (urea cycle), bilirubin, cholesterol, drug metabolites • Storage Function • Vitamins A, D, E, K and B12 • Production of bile salts • Helps in digestion
- 3. Some example of liver dysfunction • Hepatocellular disease • Cholestasis (obstruction of bile flow) • Cirrhosis • Hepatitis • Jaundice • Liver cancer • Steatosis (fatty liver) • Genetic Disorders • Hemochromatosis (iron storage)
- 4. Liver Function Tests (LFTs) • Noninvasive methods for screening of liver dysfunction • Help in identifying general types of disorder • Assess severity and allow prediction of outcome • Disease and treatment follow up
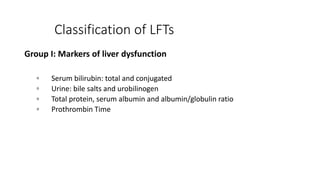
- 5. Classification of LFTs Group I: Markers of liver dysfunction ▫ Serum bilirubin: total and conjugated ▫ Urine: bile salts and urobilinogen ▫ Total protein, serum albumin and albumin/globulin ratio ▫ Prothrombin Time
- 6. Classification of LFTs Group II: Markers of hepatocellular injury ▫ Alanine aminotransferase (ALT) ▫ Aspartate aminotransferase (AST)
- 7. Classification of LFTs Group III: Markers of cholestasis ▫ Alkaline phosphatase (ALP) ▫ g-glutamyltransferase (GGT)
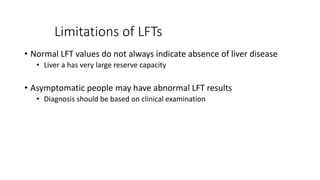
- 8. Limitations of LFTs • Normal LFT values do not always indicate absence of liver disease • Liver a has very large reserve capacity • Asymptomatic people may have abnormal LFT results • Diagnosis should be based on clinical examination
- 9. Bilirubin Bilirubin is derived from haem, an iron containing protoporphyrin mainly found in haemoglobin. An adult normally produces about 450 μmol of bilirubin daily. It is insoluble in water and is transported in plasma almost totally bound to albumin. It is taken up by liver cells and conjugated to form mono- and diglucuronides, which are much more soluble in water than unconjugated bilirubin. The conjugated bilirubin is excreted into the bile. The main functional constituents of the bile are the bile salts, which are involved in fat digestion and absorption from the small intestine.
- 10. In the terminal ileum and colon the bilirubin conjugates are attacked by bacteria to form a group of compounds that are known collectively as stercobilinogen, most of which are excreted in faeces. Some are absorbed and eventually re-excreted from the body by way of bile (the enterohepatic circulation). Small amounts of these tetrapyrroles are found in urine in which they are known as urobilinogen. When the biliary tract becomes blocked, bilirubin is not excreted and serum concentrations rise. The patient becomes jaundiced.
- 13. The aminotransferases (AST and ALT) The activities of two aminotransferases, AST and ALT, are widely used in clinical practice as a sensitive, albeit non-specific, index of acute damage to hepatocytes irrespective of its aetiology. Causes of liver damage include hepatitis, no matter the causative agent, and toxic injury, which may accompany any one of a large number of insults to the liver, including drug overdose. Acute liver damage due to shock, severe hypoxia and acute cardiac failure is also seen.
- 14. Alkaline phosphatase (ALP) Increases in alkaline phosphatase activity in liver disease are the result of increased synthesis of the enzyme by cells lining the bile canaliculi, usually in response to cholestasis, which may be either intra- or extrahepatic. Cholestasis, even of short duration, results in an increased enzyme activity to at least twice the upper end of the reference interval. High alkaline phosphatase activity may also occur when space- occupying lesions (e.g. tumors) are present. It also occurs in cirrhosis. Liver is not the sole source of alkaline phosphatase activity. Substantial amounts are present in bone, small intestine, placenta and kidney. Placental alkaline phosphatase appears in the maternal blood in the third trimester of pregnancy. Occasionally, the cause of a raised alkaline phosphatase will not be immediately apparent. The liver and bone isoenzymes can be separated by electrophoresis. However, an elevated γGT would suggest that the liver is the source of the increased alkaline phosphatase.
- 15. Gamma-glutamyl transpeptidase (γGT) γGT is a microsomal enzyme that is widely distributed in tissues including liver and renal tubules. The activity of γGT in plasma is raised whenever there is cholestasis, and it is a very sensitive index of liver pathology. It is also affected by ingestion of alcohol, even in the absence of recognizable liver disease. Alcohol and drugs such as phenytoin induce enzyme activity.
- 16. Plasma proteins Albumin is the major protein product of the liver. It has a long biological half-life in plasma (about 20 days), and therefore significant falls in albumin concentration are slow to occur if synthesis is suddenly reduced. Hypoalbuminemia is a feature of advanced chronic liver disease. It can also occur in severe acute liver damage. Alpha-fetoprotein (AFP) is synthesized by the fetal liver. In normal adults it is present in plasma at low concentrations (<3 kU/L). Measurement of AFP is of value in the investigation of hepatocellular carcinoma in which serum concentrations are increased in 80–90% of cases. AFP is also used as a marker for germ cell tumors.
- 17. Prothrombin time The prothrombin time, which is a measure of the activities of certain coagulation factors made by the liver, is sometimes used as an indicator of hepatic synthetic function. Prothrombin has a very short half-life, and an increased prothrombin time may be the earliest indicator of reduced hepatic synthesis.
- 18. Jaundice Jaundice is a yellow discoloration of the skin or sclera. This is due to the presence of bilirubin in the plasma and is not usually detectable until the concentration is greater than about 50 μmol/L. Normally the bilirubin concentration in plasma is less than 21 μmol/L. It is normally conjugated with glucuronic acid to make it more soluble, and excreted in the bile. There are three main reasons why bilirubin levels in the blood may rise: Haemolysis. The increased haemoglobin breakdown produces bilirubin, which overloads the conjugating mechanism. Failure of the conjugating mechanism within the hepatocyte. Obstruction in the biliary sytem.
- 19. Both conjugated bilirubin and unconjugated bilirubin may be present in plasma. Conjugated bilirubin is water-soluble. Unconjugated bilirubin is not water-soluble and binds to albumin from which it may be transferred to other proteins such as those in cell membranes. It is neurotoxic, and if levels rise too high in neonates, permanent brain damage can occur. Jaundice may be a consequence of haemolysis, cholestasis or hepatocellular damage. In addition there are inherited disorders of bilirubin metabolism. Gilbert’s disease is the most common and causes a mild unconjugated hyperbilirubinemia because of defective hepatic uptake of bilirubin. In this condition bilirubin levels rise on fasting.
- 20. Haemolysis Increased bilirubin production caused by haemolysis gives a predominantly unconjugated hyperbilirubinemia. This, in combination with immature liver function, is commonly encountered in babies. A rapidly rising bilirubin in a neonate should be carefully monitored as it may give rise to brain damage (kernicterus). Extrahepatic biliary obstruction Gallstones can partially or fully block the bile duct. Such a blockage is known as extrahepatic obstruction. If the blockage is complete, both bilirubin and alkaline phosphatase are raised. There is little or no urobilinogen in urine. Stools will be pale in color.
- 21. Hepatocellular damage Obstruction may be secondary to damage to the hepatocytes by infection or toxins, rather than damage to the biliary tract. The most common causes of acute jaundice seen in adults are viral hepatitis and paracetamol poisoning. In these cases, not only are the bilirubin and alkaline phosphatase levels raised, but AST and ALT are elevated indicating hepatocellular damage.
- 24. Serum bilirubin levels • Normal • 0.2 – 0.8 mg/dL • Unconjugated (indirect): • 0.2 – 0.7 mg/dL • Conjugated (direct): • 0.1 – 0.4 mg/dL • Latent jaundice: • Above 1 mg/dL • Jaundice: • Above 2 mg/dL