CCRN Review Part 1 (of 2)
- 1. CCRN REVIEW PART 1 “Never let what you cannot do interfere with what you can do” - John Wooden - Sherry L. Knowles, RN, CCRN, CRNI
- 2. CCRN REVIEW PART 1 TOPICS Acute Coronary Syndromes ARDS Acute Myocardial Infarction Chronic Lung Disease Heart Blocks Drowning Heart Failure Pneumonia Cardiac Alterations Pneumothorax Aortic Aneurysms Pulmonary Embolism Cardiomyopathy Respiratory Failure Shock States Gastrointestinal Alterations Peripheral Vascular Disease GI Bleeding Hemodynamics Pancreatitis
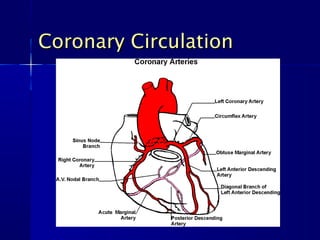
- 3. CCRN REVIEW PART 1 OBJECTIVES 1. Understand the different types of acute coronary syndromes. 2. Identify basic coronary circulation and how it relates to different types of myocardial infarctions. 3. Anticipate potential complications associated with an AMI. 4. Identify the standard treatment of an AMI. 5. Distinguish between various AV blocks. 6. Recognize the signs & symptoms of heart failure. 7. Identify the treatment of heart failure. 8. Recognize the general definition and classifications of aortic aneurysms. 9. Understand the different types of aortic dissections. 10. Recognize the signs & symptoms of cardiomyopathy. 11. Differentiate between the different types of cardiomyopathy. 12. Identify the treatment for the different types of cardiomyopathy.
- 4. CCRN REVIEW PART 1 OBJECTIVES 13. Understand the different stages of shock. 14. Differentiate between different types of shock. 15. Distinguish between arterial and venous peripheral vascular disease. 16. Identify the various treatments for peripheral vascular disease. 17. Define respiratory failure. 18. Identify the various treatments for acute respiratory failure. 19. Recognize the signs & symptoms and causes of various respiratory alterations. 20. Identify the standard treatment for various respiratory alterations. 21. Explain the common causes of gastrointestinal bleeding. 22. Describe the most commonly seen treatments for GI bleeding. 23. Describe the signs & symptoms of acute pancreatitis and available treatments.
- 5. Cardiovascular Conditions Acute Coronary Cardiomyopathy Syndromes Acute MI Heart Blocks Aortic Aneurysms Heart Failure Cardiac Alterations Shock States
- 6. Acute Coronary Syndrome DEFINITIONS – Term used to cover a group of symptoms compatible with acute myocardial ischemia – Acute myocardial ischemia is insufficient blood supply to the heart muscle usually resulting from coronary artery disease
- 7. Acute Myocardial Infarction DEFINITION – Infarction occurs due to mechanical obstruction of a coronary artery (or branch) caused by a thrombus, plaque rupture, coronary spasm and/or dissection. – STEMI vs. NSTEMI (non-STEMI)
- 8. Acute Myocardial Infarction SIGNS & SYMPTOMS – Complains Vary May include crushing chest pain (which may or may not radiate), back, neck, jaw, teeth and/or epigastric pain, SOB, nausea/vomiting and dizziness – ST elevations on ECG – Elevated cardiac enzymes
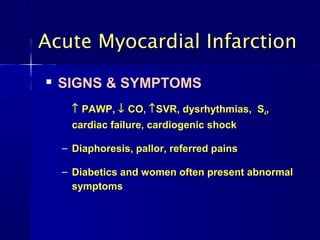
- 9. Acute Myocardial Infarction SIGNS & SYMPTOMS ↑ PAWP, ↓ CO, ↑ SVR, dysrhythmias, S4, cardiac failure, cardiogenic shock – Diaphoresis, pallor, referred pains – Diabetics and women often present abnormal symptoms
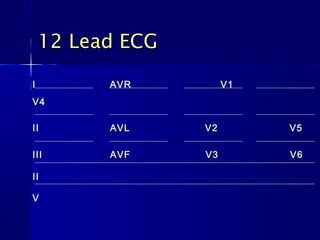
- 11. 12 Lead ECG I AVR V1 V4 II AVL V2 V5 III AVF V3 V6 II V
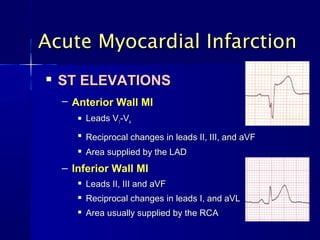
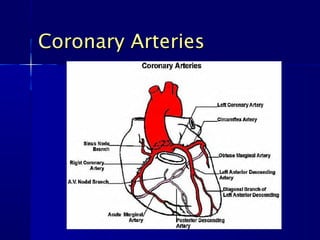
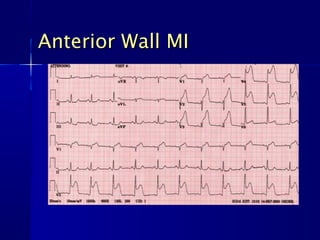
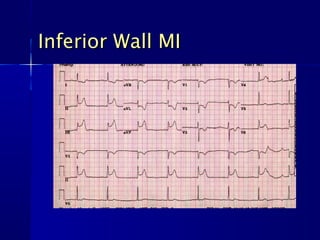
- 12. Acute Myocardial Infarction ST ELEVATIONS – Anterior Wall MI Leads V1-V4 Reciprocal changes in leads II, III, and aVF Area supplied by the LAD – Inferior Wall MI Leads II, III and aVF Reciprocal changes in leads I, and aVL Area usually supplied by the RCA
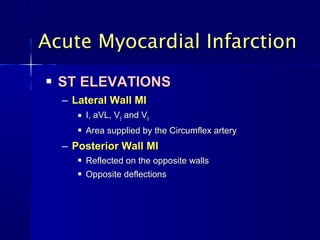
- 13. Acute Myocardial Infarction ST ELEVATIONS – Lateral Wall MI I, aVL, V5 and V6 Area supplied by the Circumflex artery – Posterior Wall MI Reflected on the opposite walls Opposite deflections
- 15. Anterior Wall MI
- 16. Inferior Wall MI
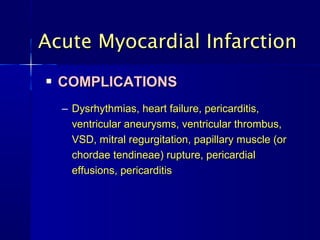
- 17. Acute Myocardial Infarction COMPLICATIONS – Dysrhythmias, heart failure, pericarditis, ventricular aneurysms, ventricular thrombus, VSD, mitral regurgitation, papillary muscle (or chordae tendineae) rupture, pericardial effusions, pericarditis
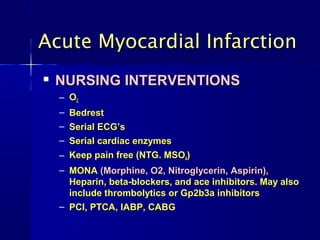
- 18. Acute Myocardial Infarction NURSING INTERVENTIONS – O2 – Bedrest – Serial ECG’s – Serial cardiac enzymes – Keep pain free (NTG. MSO4) – MONA (Morphine, O2, Nitroglycerin, Aspirin), Heparin, beta-blockers, and ace inhibitors. May also include thrombolytics or Gp2b3a inhibitors – PCI, PTCA, IABP, CABG
- 19. Acute Myocardial Infarction TREATMENT – Time Is Heart Muscle – Prompt ECG – Goals: Relieve pain, limit the size of the infarction and to prevent complications (primarily lethal dysrhythmias)
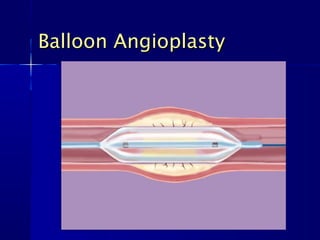
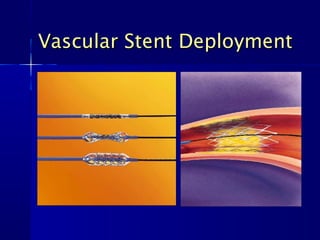
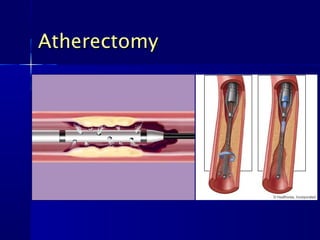
- 20. Acute Myocardial Infarction TREATMENT – MONA (Morphine, O2, Nitroglycerin, Aspirin), Heparin, beta-blockers, and ace inhibitors. May also include thrombolytics or Gp2b3a inhibitors – Cardiac Catheterization (with angioplasty, atherectomy and/or stent) – IABP, CABG, education
- 23. Atherectomy
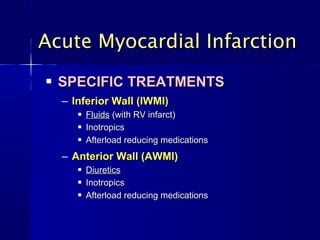
- 24. Acute Myocardial Infarction SPECIFIC TREATMENTS – Inferior Wall (IWMI) Fluids (with RV infarct) Inotropics Afterload reducing medications – Anterior Wall (AWMI) Diuretics Inotropics Afterload reducing medications
- 25. Aortic Aneurysms DEFINITION – A bulge or ballooning of the aorta When the walls of the aneurysm include all three layers of the artery, they are called true aneurysms When the wall of the aneurysm include only the outer layer, it is called a pseudo-aneurysm – May be thoracic or abdominal
- 26. Aortic Aneurysms CAUSES Atherosclerosis Marfan syndrome Hypertension Crack cocaine usage Smoking Trauma
- 27. Aortic Aneurysms Rupture An aortic aneurysm, depending on its size, may rupture, causing life-threatening internal bleeding The risk of an aneurysm rupturing increases as the aneurysm gets larger The risk of rupture also depends on the location of the aneurysm Each year, approximately 15,000 Americans die of a ruptured aortic aneurysm.
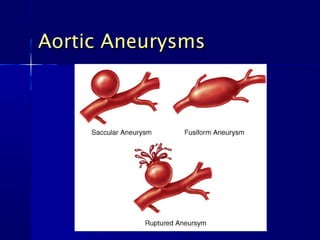
- 28. Aortic Aneurysms CLASSIFICATIONS – Classified by shape, location along the aorta, and how they are formed – May be symmetrical in shape (fusiform) or a localized weakness of the arterial wall (saccular)
- 29. Aortic Aneurysms
- 30. Aortic Aneurysms SIGNS & SYMPTOMS – Often produces no symptoms – If an aortic aneurysm suddenly ruptures it presents with extreme abdominal or back pain, a pulsating mass in the abdomen, and a drastic drop in blood pressure – An increase in the size of an aneurysm means an increased in the risk of rupture
- 31. Aortic Aneurysms THORACIC SIGNS & SYMPTOMS – Back, shoulder or neck pain – Cough, due to pressure placed on the trachea – Hoarseness – Strider, dyspnea – Difficulty swallowing – Swelling in the neck or arms
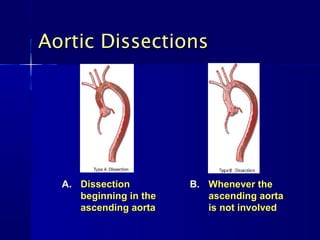
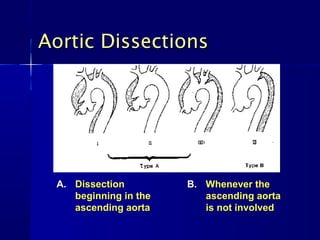
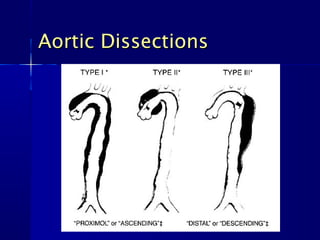
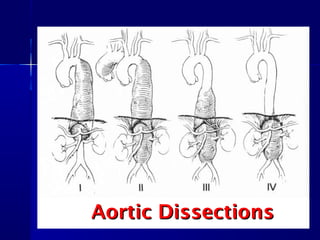
- 32. Aortic Dissections DEFINITION – Tearing of the inner layer of the aortic wall, which allows blood to leak into the wall itself and causes the separation of the inner and outer layers – Usually associated with severe chest pain radiating to the back
- 33. Aortic Dissections A. Dissection B. Whenever the beginning in the ascending aorta ascending aorta is not involved
- 34. Aortic Dissections A. Dissection B. Whenever the beginning in the ascending aorta ascending aorta is not involved
- 37. Aortic Aneurysms COMPLICATIONS Rupture Peripheral embolization Infection Spontaneous occlusion of aorta
- 38. Aortic Aneurysms TREATMENT Medical management – Controlled BP (within specific range) Surgical repair > 4.5 cm in Marfan patients or > 5 cm in non- Marfan patients will require surgical correction or endovascular stent placement
- 39. Cardiomyopathy DEFINITION – Diseases of the heart muscle that cause deterioration of the function of the myocardium
- 40. Cardiomyopathy CLASSIFICATIONS – Primary / Idiopathic (intrinsic) Heart disease of unknown cause, although viral infection and autoimmunity are suspected causes – Secondary (extrinsic) Heart disease as a result of other systemic diseases, such as autoimmune diseases, CAD, valvular disease, severe hypertension, or alcohol abuse
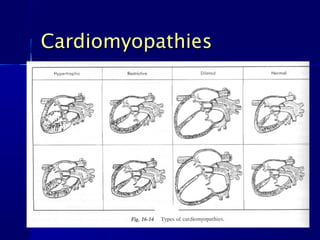
- 41. Cardiomyopathy Hypertropic Cardiomyopathy Restrictive Cardiomyopathy Dilated Cardiomyopathy
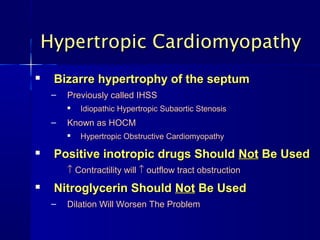
- 42. Hypertropic Cardiomyopathy Bizarre hypertrophy of the septum – Previously called IHSS Idiopathic Hypertropic Subaortic Stenosis – Known as HOCM Hypertropic Obstructive Cardiomyopathy Positive inotropic drugs Should Not Be Used ↑ Contractility will ↑ outflow tract obstruction Nitroglycerin Should Not Be Used – Dilation Will Worsen The Problem
- 43. Harley
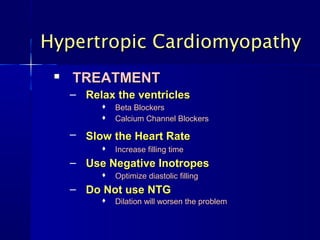
- 44. Hypertropic Cardiomyopathy TREATMENT – Relax the ventricles Beta Blockers Calcium Channel Blockers – Slow the Heart Rate Increase filling time – Use Negative Inotropes Optimize diastolic filling – Do Not use NTG Dilation will worsen the problem
- 45. Restrictive Cardiomyopathy Rigid Ventricular Wall – Due to endomyocardial fibrosis – Obstructs ventricular filling Least common form
- 46. Restrictive Cardiomyopathy TREATMENT – Positive Inotropics – Diuretics – Low Sodium Diet
- 47. Dilated Cardiomyopathy Grossly dilated ventricles without hypertrophy – Global left ventricular dysfunction – Leads to pooling of blood and embolic episodes – Leads to refractory heart failure – Leads to papillary muscle dysfunction secondary to LV dilation
- 48. Dilated Cardiomyopathy TREATMENT – Positive Inotropes – Afterload Reducers – Anticoagulants with Atrial Fib
- 49. Cardiomyopathies
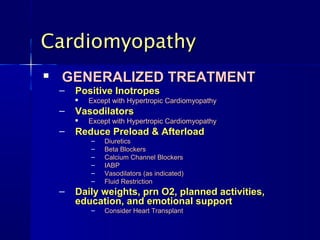
- 50. Cardiomyopathy GENERALIZED TREATMENT – Positive Inotropes Except with Hypertropic Cardiomyopathy – Vasodilators Except with Hypertropic Cardiomyopathy – Reduce Preload & Afterload – Diuretics – Beta Blockers – Calcium Channel Blockers – IABP – Vasodilators (as indicated) – Fluid Restriction – Daily weights, prn O2, planned activities, education, and emotional support – Consider Heart Transplant
- 51. CCRN REVIEW PART 1 BREAK!
- 52. Conduction Defects STABLE VS UNSTABLE – Stable Start with medications – Unstable Shock (cardioversion or defibrillation)
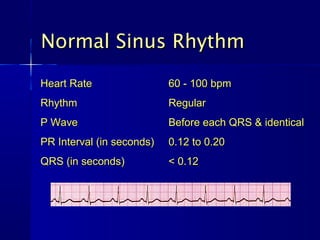
- 53. Normal Sinus Rhythm Heart Rate 60 - 100 bpm Rhythm Regular P Wave Before each QRS & identical PR Interval (in seconds) 0.12 to 0.20 QRS (in seconds) < 0.12
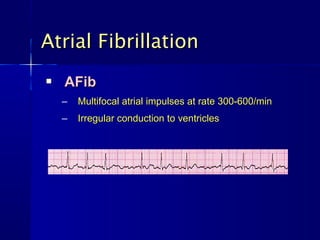
- 54. Atrial Fibrillation AFib – Multifocal atrial impulses at rate 300-600/min – Irregular conduction to ventricles
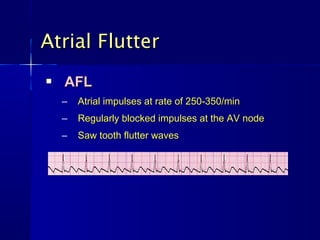
- 55. Atrial Flutter AFL – Atrial impulses at rate of 250-350/min – Regularly blocked impulses at the AV node – Saw tooth flutter waves
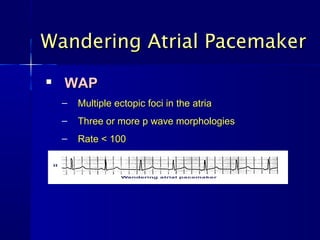
- 56. Wandering Atrial Pacemaker WAP – Multiple ectopic foci in the atria – Three or more p wave morphologies – Rate < 100
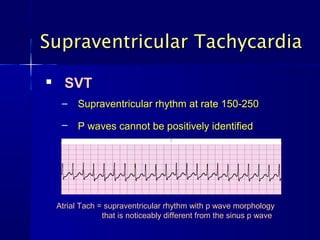
- 57. Supraventricular Tachycardia SVT – Supraventricular rhythm at rate 150-250 – P waves cannot be positively identified Atrial Tach = supraventricular rhythm with p wave morphology that is noticeably different from the sinus p wave
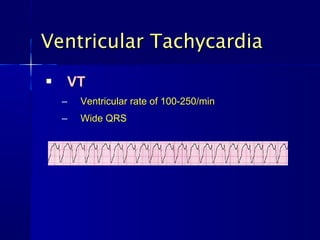
- 58. Ventricular Tachycardia VT – Ventricular rate of 100-250/min – Wide QRS
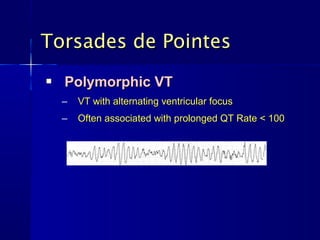
- 59. Torsades de Pointes Polymorphic VT – VT with alternating ventricular focus – Often associated with prolonged QT Rate < 100
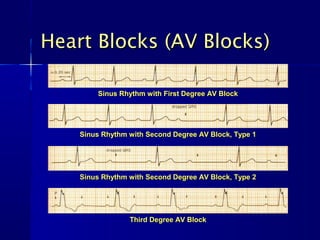
- 60. Heart Blocks (AV Blocks) Sinus Rhythm with First Degree AV Block Sinus Rhythm with Second Degree AV Block, Type 1 Sinus Rhythm with Second Degree AV Block, Type 2 Third Degree AV Block
- 61. Heart Failure DEFINITION – A condition in which the heart cannot pump sufficient blood to meet the metabolic needs of the body – Pulmonary (LVF) and/or systemic (RVF) congestion is present.
- 62. Heart Failure DEFINITION – Pulmonary Edema Fluid in the alveolus that impairs gas exchange by altering the diffusion between alveolus and capillary Acute left ventricular failure causes cardiogenic pulmonary edema Non-cardiogenic pulmonary edema is a synonym for Adult Respiratory Distress Syndrome (ARDS)
- 63. Heart Failure COMPENSATORY MECHANISMS – Sympaththetic nervous system stimulation Tachycardia Vasoconstriction and increased SVR – Renin-angiotensin-aldosterone system activation Hypo perfusion to the kidneys (renin) Vasoconstriction (angiotension) Sodium and water retention (kidneys) Ventricular dilation
- 64. Heart Failure FUNCTIONAL CLASSIFICATIONS – Class I (without noticeable limitations) – Class II (symptoms upon activity) – Class III (severe symptoms upon activity) – Class IV (symptoms at rest)
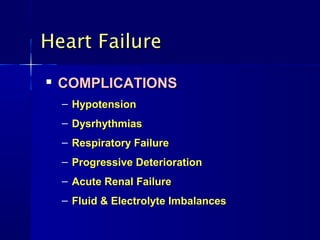
- 65. Heart Failure COMPLICATIONS – Hypotension – Dysrhythmias – Respiratory Failure – Progressive Deterioration – Acute Renal Failure – Fluid & Electrolyte Imbalances
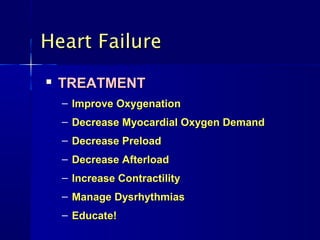
- 66. Heart Failure TREATMENT – Improve Oxygenation – Decrease Myocardial Oxygen Demand – Decrease Preload – Decrease Afterload – Increase Contractility – Manage Dysrhythmias – Educate!
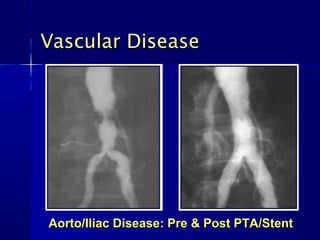
- 67. Vascular Disease Aorto/Iliac Disease: Pre & Post PTA/Stent
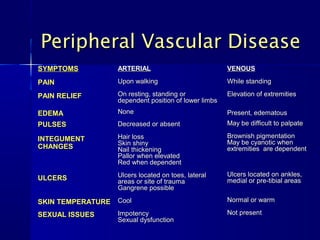
- 68. Peripheral Vascular Disease SYMPTOMS ARTERIAL VENOUS PAIN Upon walking While standing PAIN RELIEF On resting, standing or Elevation of extremities dependent position of lower limbs EDEMA None Present, edematous PULSES Decreased or absent May be difficult to palpate INTEGUMENT Hair loss Brownish pigmentation Skin shiny May be cyanotic when CHANGES Nail thickening extremities are dependent Pallor when elevated Red when dependent Ulcers located on toes, lateral Ulcers located on ankles, ULCERS areas or site of trauma medial or pre-tibial areas Gangrene possible SKIN TEMPERATURE Cool Normal or warm SEXUAL ISSUES Impotency Not present Sexual dysfunction
- 69. Peripheral Vascular Disease TREATMENTS – Medical Are they taking ASA, Coumadin, Ticlid, Plavix, Oral Contraceptives, Hormones? – Invasive PTA, atherectomy, stents – Surgical Grafts
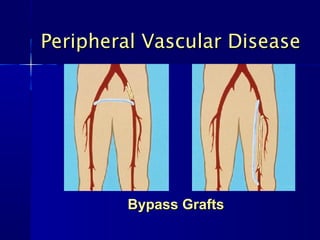
- 70. Peripheral Vascular Disease Bypass Grafts
- 71. Shock DEFINITION – Inadequate perfusion to the body tissues – Low blood pressure with impaired perfusion to the end organs – May result in multiple organ dysfunction
- 72. Shock TYPES OF SHOCK – Hypovolemic Shock – Cardiogenic Shock – Distributive Shock – Obstructive Shock
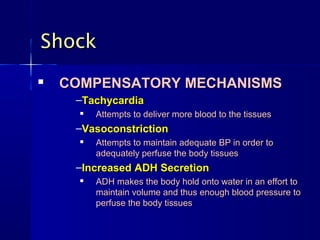
- 73. Shock COMPENSATORY MECHANISMS –Tachycardia Attempts to deliver more blood to the tissues –Vasoconstriction Attempts to maintain adequate BP in order to adequately perfuse the body tissues –Increased ADH Secretion ADH makes the body hold onto water in an effort to maintain volume and thus enough blood pressure to perfuse the body tissues
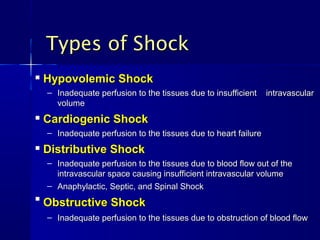
- 74. Types of Shock Hypovolemic Shock – Inadequate perfusion to the tissues due to insufficient intravascular volume Cardiogenic Shock – Inadequate perfusion to the tissues due to heart failure Distributive Shock – Inadequate perfusion to the tissues due to blood flow out of the intravascular space causing insufficient intravascular volume – Anaphylactic, Septic, and Spinal Shock Obstructive Shock – Inadequate perfusion to the tissues due to obstruction of blood flow
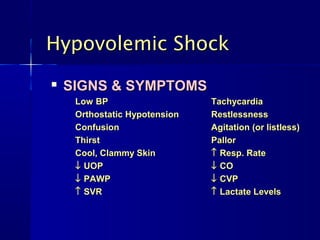
- 75. Hypovolemic Shock SIGNS & SYMPTOMS Low BP Tachycardia Orthostatic Hypotension Restlessness Confusion Agitation (or listless) Thirst Pallor Cool, Clammy Skin ↑ Resp. Rate ↓ UOP ↓ CO ↓ PAWP ↓ CVP ↑ SVR ↑ Lactate Levels
- 76. Hypovolemic Shock TREATMENT –Volume (IVF, Blood)
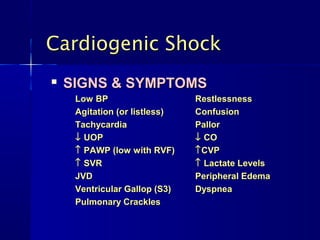
- 77. Cardiogenic Shock SIGNS & SYMPTOMS Low BP Restlessness Agitation (or listless) Confusion Tachycardia Pallor ↓ UOP ↓ CO ↑ PAWP (low with RVF) ↑ CVP ↑ SVR ↑ Lactate Levels JVD Peripheral Edema Ventricular Gallop (S3) Dyspnea Pulmonary Crackles
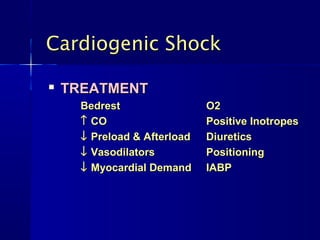
- 78. Cardiogenic Shock TREATMENT Bedrest O2 ↑ CO Positive Inotropes ↓ Preload & Afterload Diuretics ↓ Vasodilators Positioning ↓ Myocardial Demand IABP
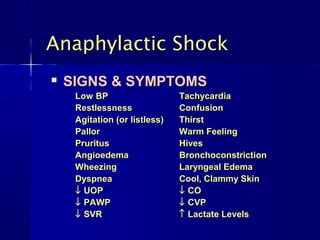
- 79. Anaphylactic Shock SIGNS & SYMPTOMS Low BP Tachycardia Restlessness Confusion Agitation (or listless) Thirst Pallor Warm Feeling Pruritus Hives Angioedema Bronchoconstriction Wheezing Laryngeal Edema Dyspnea Cool, Clammy Skin ↓ UOP ↓ CO ↓ PAWP ↓ CVP ↓ SVR ↑ Lactate Levels
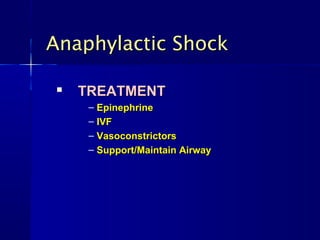
- 80. Anaphylactic Shock TREATMENT – Epinephrine – IVF – Vasoconstrictors – Support/Maintain Airway
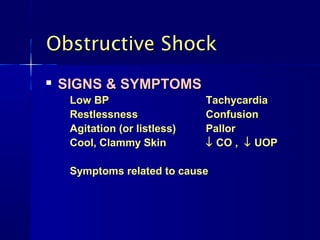
- 81. Obstructive Shock SIGNS & SYMPTOMS Low BP Tachycardia Restlessness Confusion Agitation (or listless) Pallor Cool, Clammy Skin ↓ CO , ↓ UOP Symptoms related to cause
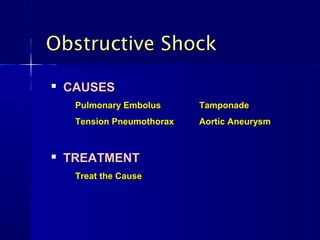
- 82. Obstructive Shock CAUSES Pulmonary Embolus Tamponade Tension Pneumothorax Aortic Aneurysm TREATMENT Treat the Cause
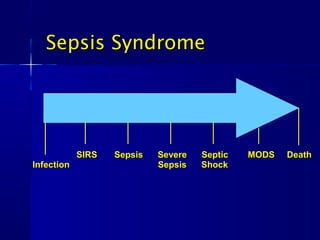
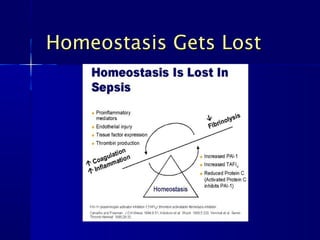
- 83. Sepsis Syndrome SIRS Sepsis Severe Septic MODS Death Infection Sepsis Shock
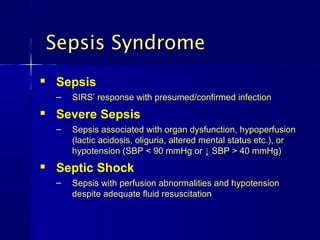
- 84. Sepsis Syndrome Sepsis – SIRS’ response with presumed/confirmed infection Severe Sepsis – Sepsis associated with organ dysfunction, hypoperfusion (lactic acidosis, oliguria, altered mental status etc.), or hypotension (SBP < 90 mmHg or ↓ SBP > 40 mmHg) Septic Shock – Sepsis with perfusion abnormalities and hypotension despite adequate fluid resuscitation
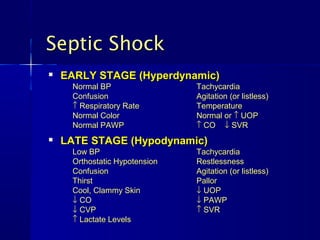
- 85. Septic Shock EARLY STAGE (Hyperdynamic) Normal BP Tachycardia Confusion Agitation (or listless) ↑ Respiratory Rate Temperature Normal Color Normal or ↑ UOP Normal PAWP ↑ CO ↓ SVR LATE STAGE (Hypodynamic) Low BP Tachycardia Orthostatic Hypotension Restlessness Confusion Agitation (or listless) Thirst Pallor Cool, Clammy Skin ↓ UOP ↓ CO ↓ PAWP ↓ CVP ↑ SVR ↑ Lactate Levels
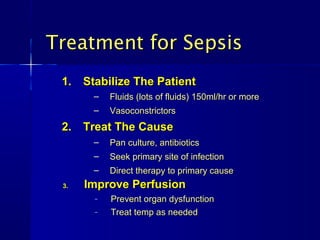
- 87. Treatment for Sepsis 1. Stabilize The Patient – Fluids (lots of fluids) 150ml/hr or more – Vasoconstrictors 2. Treat The Cause – Pan culture, antibiotics – Seek primary site of infection – Direct therapy to primary cause 3. Improve Perfusion – Prevent organ dysfunction – Treat temp as needed
- 88. HEMODYNAMICS
- 89. Invasive PA Catheter Contraindications Mechanical Tricuspid or Pulmonary Valve Right Heart Mass (thrombus and/or tumor) Tricuspid or Pulmonary Valve Endocarditis
- 90. Basic Concepts CO = HR X SV BP = CO x SVR CO and SVR are inversely related CO and SVR will change before BP changes
- 91. Stroke Volume Components Stroke Volume – Preload: the volume of blood in the ventricles at end diastole and the stretch placed on the muscle fibers – Afterload: the resistance the ventricles must overcome to eject it’s volume of blood – Contractility: the force with which the heart muscle contracts (myocardial compliance)
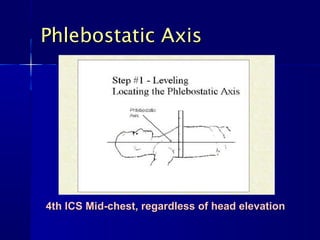
- 93. Phlebostatic Axis 4th ICS Mid-chest, regardless of head elevation
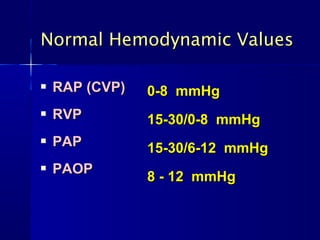
- 94. Normal Hemodynamic Values RAP (CVP) 0-8 mmHg RVP 15-30/0-8 mmHg PAP 15-30/6-12 mmHg PAOP 8 - 12 mmHg
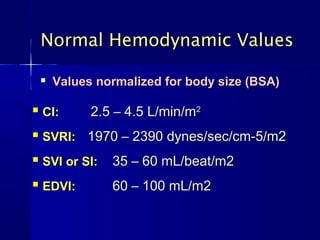
- 95. Normal Hemodynamic Values Values normalized for body size (BSA) CI: 2.5 – 4.5 L/min/m2 SVRI: 1970 – 2390 dynes/sec/cm-5/m2 SVI or SI: 35 – 60 mL/beat/m2 EDVI: 60 – 100 mL/m2
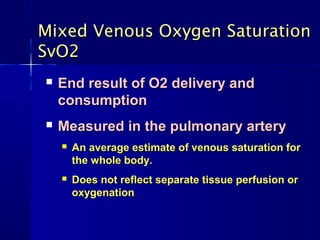
- 96. Mixed Venous Oxygen Saturation SvO2 End result of O2 delivery and consumption Measured in the pulmonary artery An average estimate of venous saturation for the whole body. Does not reflect separate tissue perfusion or oxygenation
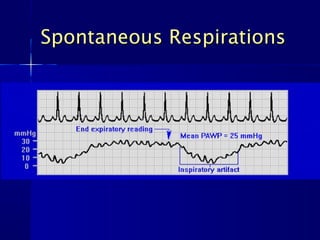
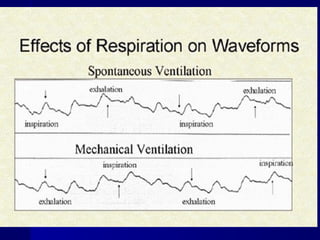
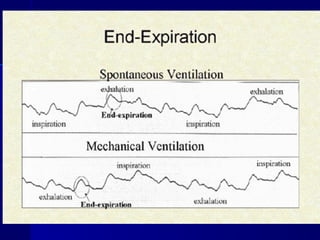
- 97. Measuring PA Pressures Measure All Hemodynamic Values at End-Expiration – “ Patient Peak” – “ Vent Valley”
- 98. Measuring PA Pressures Measure all pressures at end-expiration At bottom curve with mechanical ventilator – “Vent-Valley” Intrathoracic pressure increases during positive pressure ventilations (inspiration) – Positive deflection on waveforms Intrathoracic pressure decreases during positive pressure expiration – Negative deflection on waveforms
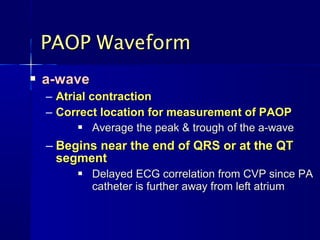
- 102. PAOP Waveform a-wave – Atrial contraction – Correct location for measurement of PAOP Average the peak & trough of the a-wave – Begins near the end of QRS or at the QT segment Delayed ECG correlation from CVP since PA catheter is further away from left atrium
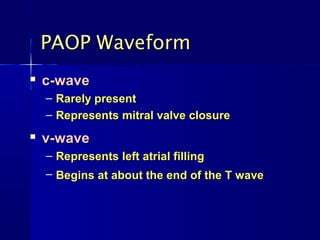
- 103. PAOP Waveform c-wave – Rarely present – Represents mitral valve closure v-wave – Represents left atrial filling – Begins at about the end of the T wave
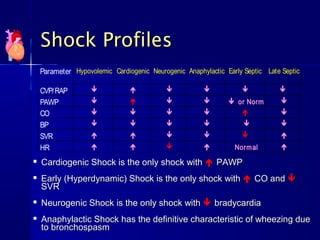
- 104. Shock Profiles Parameter Hypovolemic Cardiogenic Neurogenic Anaphylactic Early Septic Late Septic CVP/RAP PAWP or Norm CO BP SVR HR Norm al Cardiogenic Shock is the only shock with PAWP Early (Hyperdynamic) Shock is the only shock with CO and SVR Neurogenic Shock is the only shock with bradycardia Anaphylactic Shock has the definitive characteristic of wheezing due to bronchospasm
- 105. CCRN REVIEW PART 1 BREAK!
- 106. Respiratory Alterations ARDS Chronic Lung Disease Drowning Pneumonia Pneumothorax Pulmonary Respiratory Embolism Failure
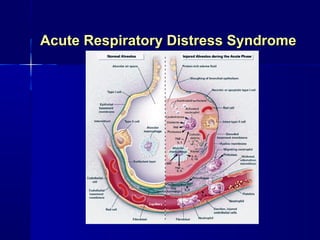
- 107. ARDS DEFINITIONS – Severe respiratory failure associated with pulmonary infiltrates (similar to infant hyaline membrane disease) – Pulmonary edema in the absence of fluid overload or depressed LV function (Non-cardiogenic pulmonary edema) – Originates from a number of insults involving damage to the alveolar-capillary membrane
- 108. Acute Respiratory Distress Syndrome
- 109. ARDS PATHOPHYSIOLOGY – Inflammatory mediators are released causing extensive structural damage – Increased permeability of pulmonary microvasculature causes leakage of proteinaceous fluid across the alveolar– capillary membrane – Also causes damage to the surfactant-producing type II cells
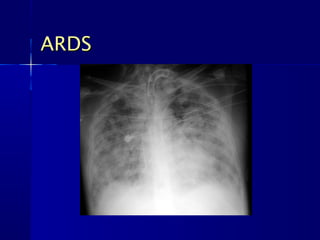
- 110. ARDS CXR CHARACTERISTICS – Normal size heart – No pleural effusion – Ground Glass appearance – Often normal early in the disease but may rapidly progress to complete whiteout
- 111. ARDS
- 112. ARDS SIGNS & SYMPTOMS – Symptoms develop 24 to 48 hours of injury Sudden progressive disorder Pulmonary edema Severe dyspnea Hypoxemia REFRACTORY to O2 Decreased lung compliance Diffuse pulmonary infiltrates – Symptoms may be minimal compared to CXR – Rales may be heard
- 113. ARDS RISK FACTORS Common Risk Other Risk Factors Factors Sepsis Smoke inhalation Acute Pancreatitis Massive Inhaled toxins DIC Trauma Burns Head Injury Shock Near Drowning ↑ ICP Multiple DKA Fat Emboli Transfusions Pregnancy Blood Products Pneumonia Eclampsia Heart/Lung Bypass Aspiration Amniotic Fluid Embolus Tumor Lysis Infection Drugs Pulmonary Contusion Narcotics
- 114. ARDS TREATMENT – Respiratory Support – PEEP, CPAP
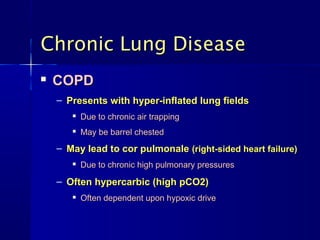
- 115. Chronic Lung Disease COPD – Presents with hyper-inflated lung fields Due to chronic air trapping May be barrel chested – May lead to cor pulmonale (right-sided heart failure) Due to chronic high pulmonary pressures – Often hypercarbic (high pCO2) Often dependent upon hypoxic drive
- 116. Chronic Lung Disease COPD TREATMENT – Avoid overuse of oxygen (except in emergencies) – Bronchodilators – Steroids – Hydration – Education Pursed Lip Breathing Leaning Upright
- 117. Near Drowning Salt Water – Causes body fluids to shift into lungs Osmosis: From low to high concentration Results in hemoconcentration & hypovolemia – Results in acute pulmonary edema Fresh Water – Fluids shift into body tissues Results in hemodilution & hypervolemia Can result in gross edema – Damaged alveoli fill with proteinaceous fluid May lead to pulmonary edema
- 118. Pneumonia Lung infection (bacterial, viral, or fungal) – Most commonly caused by Streptococcus pneumoniae Symptoms include fever, pleuretic chest pain, productive cough, and tachypnea – Often presents bronchial breath sounds over the lung area Treatment involves giving the right antibiotic
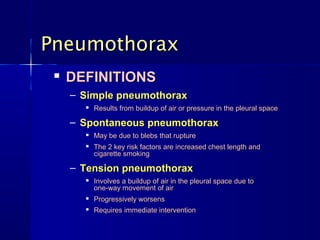
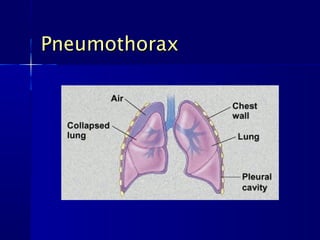
- 119. Pneumothorax DEFINITIONS – Simple pneumothorax Results from buildup of air or pressure in the pleural space – Spontaneous pneumothorax May be due to blebs that rupture The 2 key risk factors are increased chest length and cigarette smoking – Tension pneumothorax Involves a buildup of air in the pleural space due to one-way movement of air Progressively worsens Requires immediate intervention
- 120. Pneumothorax
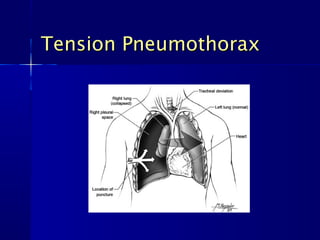
- 121. Tension Pneumothorax
- 122. Pneumothorax CAUSES – Barotrauma – Injury – Blebs
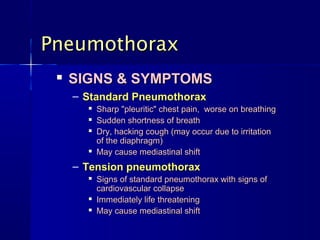
- 123. Pneumothorax SIGNS & SYMPTOMS – Standard Pneumothorax Sharp "pleuritic" chest pain, worse on breathing Sudden shortness of breath Dry, hacking cough (may occur due to irritation of the diaphragm) May cause mediastinal shift – Tension pneumothorax Signs of standard pneumothorax with signs of cardiovascular collapse Immediately life threatening May cause mediastinal shift
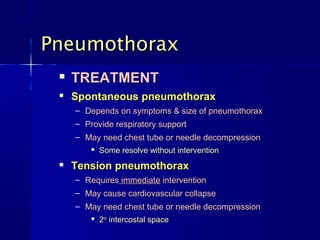
- 124. Pneumothorax TREATMENT Spontaneous pneumothorax – Depends on symptoms & size of pneumothorax – Provide respiratory support – May need chest tube or needle decompression Some resolve without intervention Tension pneumothorax – Requires immediate intervention – May cause cardiovascular collapse – May need chest tube or needle decompression 2nd intercostal space
- 125. Pneumothorax TREATMENT – Pleurodesis Chemical or surgical adhesion of the lung to the chest wall Used for multiple collapsed lungs or persistent collapse
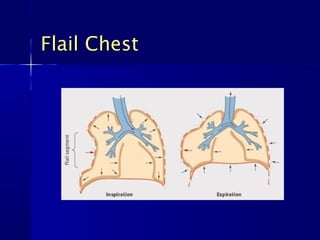
- 126. Flail Chest
- 127. Pulmonary Embolism Definition – Arterial embolus that obstructs blood flow to the lung Signs & Symptoms – Symptoms include sudden dyspnea, cough, chest pain, hemoptysis and sinus tachycardia – Blood gas shows low pO2 & low pCO2 – May present positive Homan’s Sign – May present loud S2
- 128. Pulmonary Embolism Diagnostic Tests – CXR – VQ Scan – Spiral CT – Pulmonary arteriogram – Venous ultrasound of the lower extremities – ABG with low pO2 & low pCO2 – D-Dimer
- 129. Pulmonary Embolism Treatment – Requires immediate intervention – Provide respiratory support – Treat pain & comfort – Usually includes intravenous heparin Heparin reduces risk of secondary thrombus formation while clot is reabsorbed – May require embolectomy – May require thrombolysis – May need umbrella filter – May need long term anticoagulants
- 130. Respiratory Failure DEFINITIONS – Failure to maintain adequate gas exchange – Inadequate blood oxygenation or CO2 removal – PaO2 < 50 mmHg and/or PaCO2 > 50 mmHg and/or pH < 7.35 on Room Air
- 131. Respiratory Failure TYPE I Hypoxemia without hypercapnia TYPE II Hypoxemia with hypercapnia
- 132. Respiratory Failure CAUSES – V/Q Mismatching – Intrapulmonary Shunting – Alveolar Hypoventilation
- 133. Respiratory Failure V/Q MISMATCHING – COPD – Interstitial Lung Disease – Pulmonary Embolism
- 134. Respiratory Failure PULMONARY SHUNTING – AV fistulas/malformations – Alveolar collapse (atelectasis) – Alveolar consolidation (pneumonia) – Excessive mucus accumulation
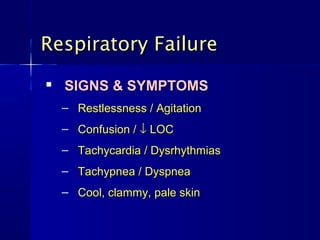
- 135. Respiratory Failure SIGNS & SYMPTOMS – Restlessness / Agitation – Confusion / ↓ LOC – Tachycardia / Dysrhythmias – Tachypnea / Dyspnea – Cool, clammy, pale skin
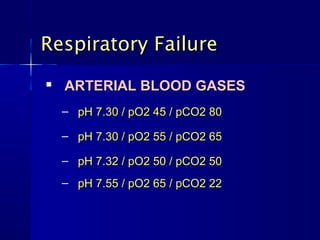
- 136. Respiratory Failure ARTERIAL BLOOD GASES – pH 7.30 / pO2 45 / pCO2 80 – pH 7.30 / pO2 55 / pCO2 65 – pH 7.32 / pO2 50 / pCO2 50 – pH 7.55 / pO2 65 / pCO2 22
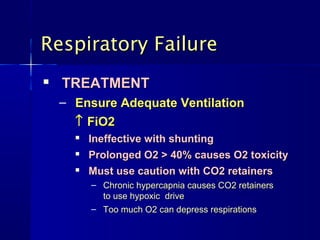
- 137. Respiratory Failure TREATMENT – Ensure Adequate Ventilation ↑ FiO2 Ineffective with shunting Prolonged O2 > 40% causes O2 toxicity Must use caution with CO2 retainers – Chronic hypercapnia causes CO2 retainers to use hypoxic drive – Too much O2 can depress respirations
- 138. CCRN REVIEW PART 1 BREAK!
- 139. Gastrointestinal Alterations GI Bleed Pancreatitis
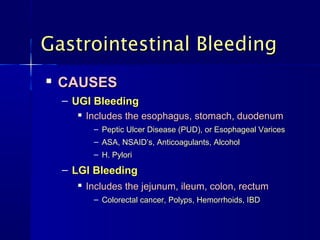
- 140. Gastrointestinal Bleeding CAUSES – UGI Bleeding Includes the esophagus, stomach, duodenum – Peptic Ulcer Disease (PUD), or Esophageal Varices – ASA, NSAID’s, Anticoagulants, Alcohol – H. Pylori – LGI Bleeding Includes the jejunum, ileum, colon, rectum – Colorectal cancer, Polyps, Hemorrhoids, IBD
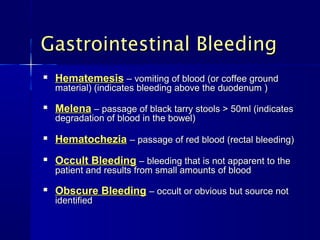
- 142. Gastrointestinal Bleeding Hematemesis – vomiting of blood (or coffee ground material) (indicates bleeding above the duodenum ) Melena – passage of black tarry stools > 50ml (indicates degradation of blood in the bowel) Hematochezia – passage of red blood (rectal bleeding) Occult Bleeding – bleeding that is not apparent to the patient and results from small amounts of blood Obscure Bleeding – occult or obvious but source not identified
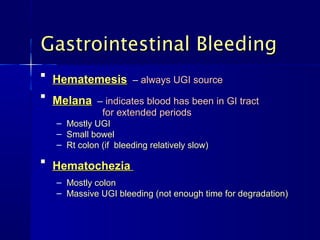
- 143. Gastrointestinal Bleeding Hematemesis – always UGI source Melana – indicates blood has been in GI tract for extended periods – Mostly UGI – Small bowel – Rt colon (if bleeding relatively slow) Hematochezia – Mostly colon – Massive UGI bleeding (not enough time for degradation)
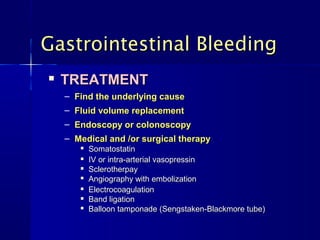
- 144. Gastrointestinal Bleeding TREATMENT – Find the underlying cause – Fluid volume replacement – Endoscopy or colonoscopy – Medical and /or surgical therapy Somatostatin IV or intra-arterial vasopressin Sclerotherpay Angiography with embolization Electrocoagulation Band ligation Balloon tamponade (Sengstaken-Blackmore tube)
- 145. The Pancreas The Pancreas secretes digestive enzymes, bicarbonate, water, and some electrolytes into the duodenum via the pancreatic duct – Lipase, Amylase, Trypsin The Pancreas also produces and secretes insulin
- 146. Pancreatitis DEFINITION – An autodigestive process resulting from premature activation of pancreatic enzymes
- 147. Pancreatitis PATHOSHYSIOLOGY • Inactive pancreatic enzymes are activated outside of the duodenum • The swelling pancreas causes fluids to shift into the retro peritoneum and bowel • Fluid shifts can cause severe hypovolemia and hypotension • Inflammation cause commotion around pancreas
- 148. Pancreatitis MANY CAUSES – Alcoholism – Hypercalcemia – Biliary Disease – Peptic Ulcer Disease – Gallstones – Cystic Fibrosis – Infections – Vascular Disease – Hyperparathyroidism – Multiple Drugs – Hypertriglyceridemia – Much Much More
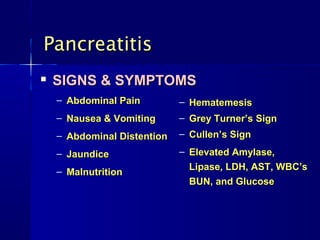
- 149. Pancreatitis SIGNS & SYMPTOMS – Abdominal Pain – Hematemesis – Nausea & Vomiting – Grey Turner’s Sign – Abdominal Distention – Cullen’s Sign – Jaundice – Elevated Amylase, – Malnutrition Lipase, LDH, AST, WBC’s BUN, and Glucose
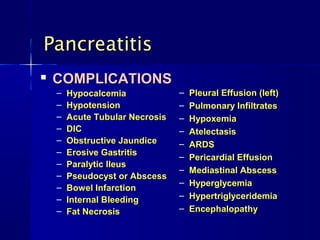
- 150. Pancreatitis COMPLICATIONS – Hypocalcemia – Pleural Effusion (left) – Hypotension – Pulmonary Infiltrates – Acute Tubular Necrosis – Hypoxemia – DIC – Atelectasis – Obstructive Jaundice – ARDS – Erosive Gastritis – Pericardial Effusion – Paralytic Ileus – Mediastinal Abscess – Pseudocyst or Abscess – Hyperglycemia – Bowel Infarction – Internal Bleeding – Hypertriglyceridemia – Fat Necrosis – Encephalopathy
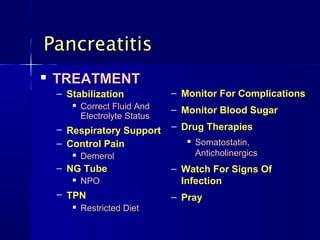
- 151. Pancreatitis TREATMENT – Stabilization – Monitor For Complications Correct Fluid And – Monitor Blood Sugar Electrolyte Status – Respiratory Support – Drug Therapies – Control Pain Somatostatin, Demerol Anticholinergics – NG Tube – Watch For Signs Of NPO Infection – TPN – Pray Restricted Diet
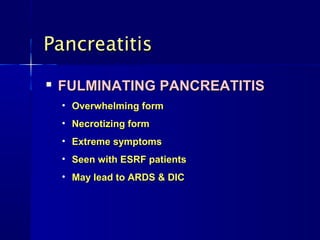
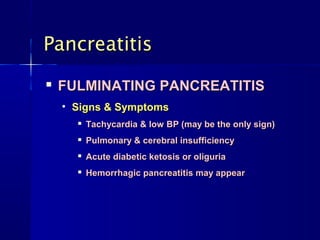
- 152. Pancreatitis FULMINATING PANCREATITIS • Overwhelming form • Necrotizing form • Extreme symptoms • Seen with ESRF patients • May lead to ARDS & DIC
- 153. Pancreatitis FULMINATING PANCREATITIS • Signs & Symptoms Tachycardia & low BP (may be the only sign) Pulmonary & cerebral insufficiency Acute diabetic ketosis or oliguria Hemorrhagic pancreatitis may appear
- 154. CCRN REVIEW THE END PART 1
- 155. CCRN REVIEW PART 1 THANK YOU
- 156. References American Heart Association. (2005). Guidelines 2005 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Available at: www.americanheart.org. Bridges EJ.(2006) Pulmonary artery pressure monitoring: when, how, and what else to use. AACN Adv Crit Care. 2006;17(3):286–303. Chulay, M., Burns S. M. (2006). AACN Essentials of Critical Care Nursing. McGraw-Hill Companies, Inc., Chapter 23. Finkelmeier, B., Marolda, D. (2004) Aortic Dissection, Journal of Cardiovascular Nursing: 15(4):15–24. Hughes E. (2004). Understanding the care of patients with acute pancreatitis. Nurs Standard: (18) pgs 45-54. Sole, M. L., Klein, D. G. & Moseley, M. (2008). Introduction to Critical Care Nursing. 5th ed. Philadelphia, Pa: Saunders. Thelan, L. A., Urden, L. D., Lough, M. E. (2006). Critical care: Diagnosis and Treatment for repair of abdominal aortic aneurysm. St. Louis, Mo.: Mosby/Elsevier. pg 145-188.
- 157. References Continued Urden, L., Lough, M. E. & Stacy, K. L. (2009). Thelan's Critical Care Nursing: Diagnosis and Management (6th ed). St. Louis, Mo.: Mosby/Elsevier. Woods, S., Sivarajan Froelicher, E. S., & Motzer, S. U. (2004). Cardiac Nursing. 5th ed. Philadelphia, Pa: Lippincott Williams & Wilkins. Wynne J, Braunwald E. (2004). The Cardiomyopathies in Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine (7th Edition). Philadelphia: W.B. Saunders, vol. 2, pps. 1659–1696, 1751–1803. Zimmerman & Sole. (2001). Critical Care Nursing (3rd Edition). WB Saunders., pgs. 41-80, 176-180, 242-266. Anderson, L. (July 2001). Abdominal Aortic Aneurysm, Journal of Cardiovascular Nursing:15(4):1–14, July 2001. Irwin, R. S.; Rippe, J. M. (January 2003). Intensive Care Medicine. Lippincott Williams & Wilkins, Philadelphia: pgs. 35-548. Wung, S., Aouizerat, B. E. (Nov/Dec 2004). Aortic Aneurysms. Journal of Cardiovascular Nursing. Lippincott Williams & Wilkins, Inc.:19(6):409-416, 34(2).