Non Invasive Ventilation Update
- 1. Dean R. Hess PhD RRT Associate Professor of Anesthesia Harvard Medical School Assistant Director of Respiratory Care Massachusetts General Hospital Editor in Chief Respiratory Care Noninvasive Ventilation: Update 2010
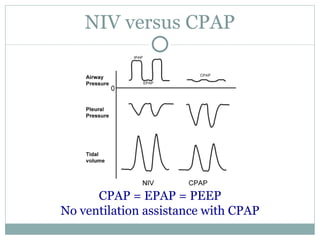
- 2. NIV versus CPAP CPAP = EPAP = PEEP No ventilation assistance with CPAP
- 3. Mask CPAP Obstructive sleep apnea Cardiogenic pulmonary edema Treat post-operative atelectasis Acute hypoxemic respiratory failure?
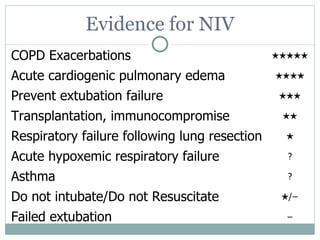
- 4. Evidence for NIV COPD Exacerbations ★★★★★ Acute cardiogenic pulmonary edema ★★★★ Prevent extubation failure ★★★ Transplantation, immunocompromise ★★ Respiratory failure following lung resection ★ Acute hypoxemic respiratory failure ? Asthma ? Do not intubate/Do not Resuscitate ★ /− Failed extubation −
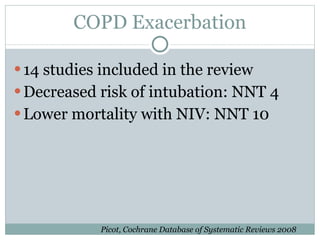
- 5. COPD Exacerbation 14 studies included in the review Decreased risk of intubation: NNT 4 Lower mortality with NIV: NNT 10 Picot, Cochrane Database of Systematic Reviews 2008
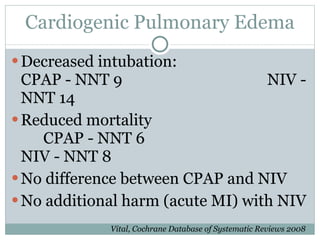
- 6. Cardiogenic Pulmonary Edema Decreased intubation: CPAP - NNT 9 NIV - NNT 14 Reduced mortality CPAP - NNT 6 NIV - NNT 8 No difference between CPAP and NIV No additional harm (acute MI) with NIV Vital, Cochrane Database of Systematic Reviews 2008
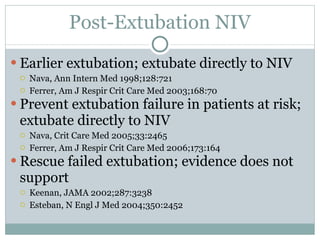
- 7. Post-Extubation NIV Earlier extubation; extubate directly to NIV Nava, Ann Intern Med 1998;128:721 Ferrer, Am J Respir Crit Care Med 2003;168:70 Prevent extubation failure in patients at risk; extubate directly to NIV Nava, Crit Care Med 2005;33:2465 Ferrer, Am J Respir Crit Care Med 2006;173:164 Rescue failed extubation; evidence does not support Keenan, JAMA 2002;287:3238 Esteban, N Engl J Med 2004;350:2452
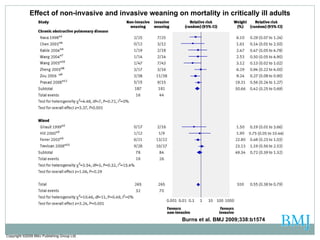
- 8. Copyright ©2009 BMJ Publishing Group Ltd. Burns et al. BMJ 2009;338:b1574 Effect of non-invasive and invasive weaning on mortality in critically ill adults
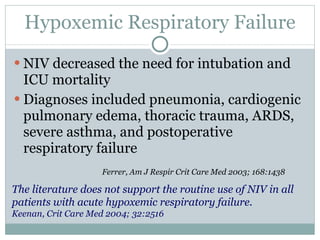
- 9. Hypoxemic Respiratory Failure NIV decreased the need for intubation and ICU mortality Diagnoses included pneumonia, cardiogenic pulmonary edema, thoracic trauma, ARDS, severe asthma, and postoperative respiratory failure Ferrer, Am J Respir Crit Care Med 2003; 168:1438 The literature does not support the routine use of NIV in all patients with acute hypoxemic respiratory failure. Keenan, Crit Care Med 2004; 32:2516
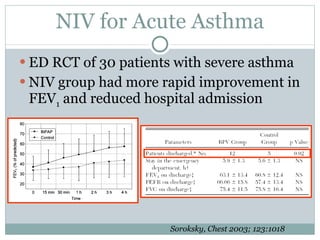
- 10. NIV for Acute Asthma ED RCT of 30 patients with severe asthma NIV group had more rapid improvement in FEV 1 and reduced hospital admission Soroksky, Chest 2003; 123:1018
- 11. 52 immunosuppressed patients with hypoxemic acute respiratory failure NIV every 3 hrs for at least 45 min Fewer patients in the NIV group than in the standard-treatment group required endotracheal intubation (12 vs. 20), died in the ICU (10 vs 18), or died in the hospital (13 vs 21) N Engl J Med 2001;344:481
- 12. Crit Care Med 2005;33:1976
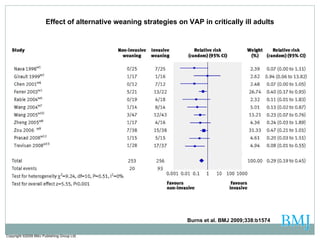
- 13. Copyright ©2009 BMJ Publishing Group Ltd. Burns et al. BMJ 2009;338:b1574 Effect of alternative weaning strategies on VAP in critically ill adults
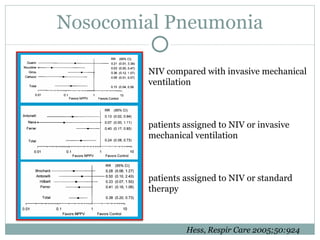
- 14. Nosocomial Pneumonia NIV compared with invasive mechanical ventilation patients assigned to NIV or invasive mechanical ventilation patients assigned to NIV or standard therapy Hess, Respir Care 2005;50:924
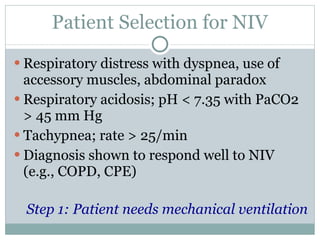
- 15. Patient Selection for NIV Respiratory distress with dyspnea, use of accessory muscles, abdominal paradox Respiratory acidosis; pH < 7.35 with PaCO2 > 45 mm Hg Tachypnea; rate > 25/min Diagnosis shown to respond well to NIV (e.g., COPD, CPE) Step 1: Patient needs mechanical ventilation
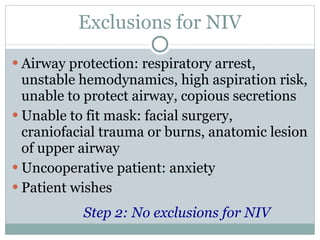
- 16. Exclusions for NIV Airway protection: respiratory arrest, unstable hemodynamics, high aspiration risk, unable to protect airway, copious secretions Unable to fit mask: facial surgery, craniofacial trauma or burns, anatomic lesion of upper airway Uncooperative patient: anxiety Patient wishes Step 2: No exclusions for NIV
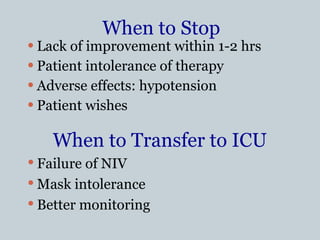
- 17. When to Stop Lack of improvement within 1-2 hrs Patient intolerance of therapy Adverse effects: hypotension Patient wishes When to Transfer to ICU Failure of NIV Mask intolerance Better monitoring
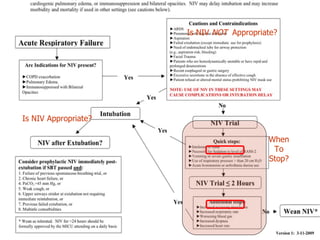
- 18. Is NIV Appropriate? Is NIV NOT Appropriate? When To Stop?
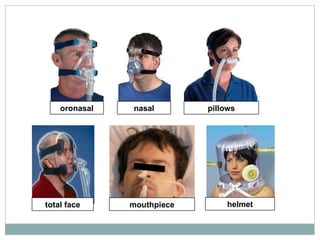
- 19. The Interface Mask Nasal Oronasal Total face Pillows Mouthpiece Helmet
- 20. nasal total face oronasal pillows mouthpiece helmet
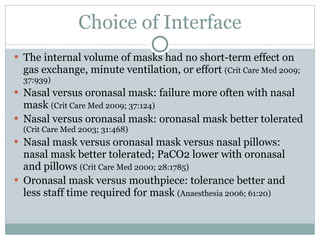
- 21. Choice of Interface The internal volume of masks had no short-term effect on gas exchange, minute ventilation, or effort (Crit Care Med 2009; 37:939) Nasal versus oronasal mask: failure more often with nasal mask (Crit Care Med 2009; 37:124) Nasal versus oronasal mask: oronasal mask better tolerated (Crit Care Med 2003; 31:468) Nasal mask versus oronasal mask versus nasal pillows: nasal mask better tolerated; PaCO2 lower with oronasal and pillows (Crit Care Med 2000; 28:1785) Oronasal mask versus mouthpiece: tolerance better and less staff time required for mask (Anaesthesia 2006; 61:20)
- 22. Mouth Leak Decreased comfort Less effective ventilation Ineffective trigger/cycle NIV failure (Soo Hoo 1994, Fraticelli 2009) Increased nasal resistance (Richards 1996) Upper airway drying (De Araujo 2000) Disrupted sleep (Meyer 1997; Tescheler 1999) Oronasal mask; coaching?; chin strap?
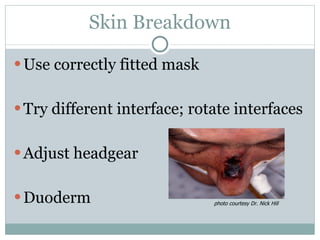
- 23. Skin Breakdown Use correctly fitted mask Try different interface; rotate interfaces Adjust headgear Duoderm photo courtesy Dr. Nick Hill
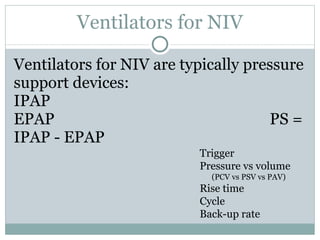
- 25. Ventilators for NIV Ventilators for NIV are typically pressure support devices: IPAP EPAP PS = IPAP - EPAP Trigger Pressure vs volume (PCV vs PSV vs PAV) Rise time Cycle Back-up rate
- 26. AVAPS: Average Volume Assured Pressure Support Estimates patient tidal volume over several breaths and compares it to target tidal volume Gradually changes IPAP (0.5 – 1 cm H 2 O/min) Similar to PRVC, Autoflow, and VS
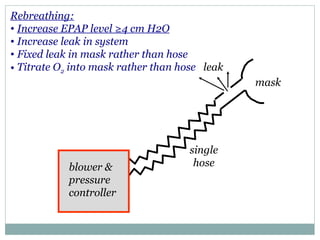
- 27. blower & pressure controller single hose leak Rebreathing: Increase EPAP level ≥4 cm H2O Increase leak in system Fixed leak in mask rather than hose Titrate O 2 into mask rather than hose mask
- 28. Inhaled Bronchodilators Nebulizer therapy inline with NIV MDI therapy inline with NIV Hess, J Aerosol Med 2007; 20:S85 Iosson, N Engl J Med 2006; 354:e8
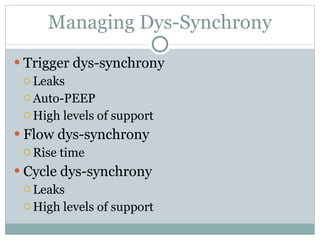
- 30. Managing Dys-Synchrony Trigger dys-synchrony Leaks Auto-PEEP High levels of support Flow dys-synchrony Rise time Cycle dys-synchrony Leaks High levels of support
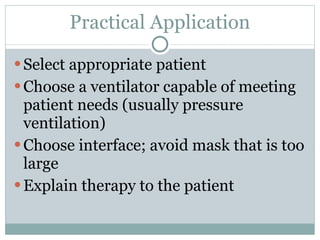
- 31. Practical Application Select appropriate patient Choose a ventilator capable of meeting patient needs (usually pressure ventilation) Choose interface; avoid mask that is too large Explain therapy to the patient
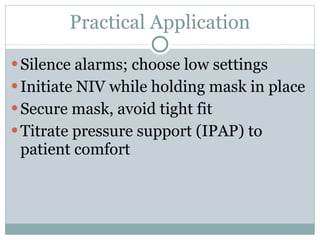
- 32. Practical Application Silence alarms; choose low settings Initiate NIV while holding mask in place Secure mask, avoid tight fit Titrate pressure support (IPAP) to patient comfort
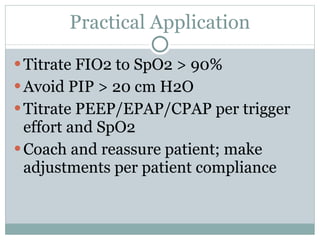
- 33. Practical Application Titrate FIO2 to SpO2 > 90% Avoid PIP > 20 cm H2O Titrate PEEP/EPAP/CPAP per trigger effort and SpO2 Coach and reassure patient; make adjustments per patient compliance
- 34. Complications Leaks Mask discomfort and facial soreness Eye irritation Sinus congestion Oronasal drying Patient-ventilator dyssynchrony Gastric insufflation Hemodynamic compromise (Complications are usually minor)
- 35. Cough Assist
- 36. NIV Success clinician skills equipment selection patient selection
Editor's Notes
- Hess, Mechanical Ventilation
- Hess, Mechanical Ventilation