Ect by dr asma
- 1. Electro-Convulsive Therapy (ECT) Dr.Asma A Rehman Consultant Psychiatrist
- 2. Overview • Definition • History • Machines • Mechanism of action • Indications • Technique • Unwanted effects • Summary
- 3. Definition • ECT is a procedure in which electric currents are passed through brain, intentionally triggering a brief seizure. • Formerly known as “ Electric Shock ” • Safe for all ages, with debilitating illness, and during pregnancy.
- 4. History • Introduced in late 1930’s • On basis of mistaken idea : “ Epilepsy and Schizophrenia do not occur together” • Induced fits should lead to improvement in Schizophrenia. • Initially chemically fits were induced by using Camphor or Pentylenetetrazol. • IV Camphor induced seizure in 1934 by Meduna As procedure was painful so Then started on ECT • IM pentylenetetrazol • 1st ECT in 1938 .
- 5. • 1940, curare was developed for use as a muscle relaxant during ECT • Succinylcholine, a depolarizing muscle relaxant, was introduced in 1951 • 1975 movie “One Flew Over the Cuckoo’s Nest,” with Jack Nicholson thrashing about, forced against his will to endure painful, violent seizures • In 1985, the National Institutes of Health and National Institute of Mental Health Consensus Conference on ECT endorsed a role for the use of ECT
- 6. ECT machines. • Four machines currently available are recommended by the College: 1. the Ectron Series 5A, 2. Ectonus (Electron Ltd, Letchworth), 3. Mecta SR2 and JR2 (Mecta Corp., Lake Oswego, OR) and 4. Thymatron-DGx (Somatics Inc., Lake Bluff, IL) ( Royal College of Psychiatrists, 1995).
- 7. ECT machine in LNH (ECTONUS)
- 9. Mechanism Of Action. • Neuro-endocrine system • Neuro-endocrine dysregulation Is prominent in Patients with Mental disorders for which ECT is effective. • In severely depressed patients, Adrenal glands produce too much Cortisol. • The high blood levels disrupts normal diurnal rhythm of other glandular discharges and the glands do not respond to usual feed back mechanism.
- 10. • The most prominent features of depression are distortion of functions regulated by Neuro-endocrine gland in self- adjusting feed back. • Each Seizure stimulates Hypothalamus to discharge its hormones, which causes Pituitary gland to discharge its products which then effects level of Cortisol. • The first effects of this cascade are Transitory, but repeated Seizures restore the normal interaction of HPA axis. • Feeding & sleeping becomes normal, followed by motor activity, mood , memory & thoughts.
- 11. • After some course of ECT, the return to normal Endocrine functions. • At other times, glands revert their abnormal activities, & mental disorder becomes evident again. • In these cases repeated stimulation of Hypothalamus & Pituitary by continuation of ECT restore & sustain normal glandular function & support normal mental state.
- 12. • Neuro-transmitter System. • Almost all neurotransmitters effected by ECT. • Down regulation of pot-synaptic beta adrenergic receptor • Increase post-synaptic receptor & change in pre-synaptic discharge.
- 13. Indications. • 1) Treatment of choice : • Severe depressive illness when associated with : oLife threatening illness bec of refusal of food & fluids. oHigh Suicidal risk. • 2) Considered for: • Severe Depressive illness associated with: oStupor. oMarked Psychomotor retardation. oDepressive delusions & hallucinations.
- 14. • 3) 2nd & 3rd line of treatment: • Depressive illness: o If not responsive to anti-depressant drugs • 4) Treatment of Mania: • associated with: o Life threatening physical exhaustion. o Not responded to appropriate drug treatment. • 5) For treatment of Acute Schizophrenia: • as 4th line treatment option. o After trial of 2 anti-psychotics & Clozapine was ineffective • 6) Catatonia. o Where treatment with Benzodiazepine ineffective.
- 15. • Mortality Rate. • 3-4/100,000 Treatments. • Due to General Medical conditions or General Anesthesia complications. • Contraindications. • No absolute contraindications. • Contraindications are due to anesthesia
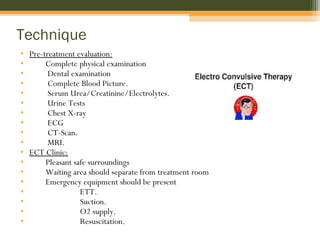
- 16. Technique • Pre-treatment evaluation: • Complete physical examination • Dental examination • Complete Blood Picture. • Serum Urea/Creatinine/Electrolytes. • Urine Tests • Chest X-ray • ECG • CT-Scan. • MRI. • ECT Clinic: • Pleasant safe surroundings • Waiting area should separate from treatment room • Emergency equipment should be present • ETT. • Suction. • O2 supply. • Resuscitation.
- 17. • Arrival of patient: • Patient should be at ease. • Check identity • Check consent form. • Check drug sheet. • Administration of Anesthesia. • NPO for at least 5 hours. • I/V access maintained. • Attach Monitor • Give Muscle relaxant • Anesthetic agent • Hyperventilation with O2 • Bite Block. • Electrode placement and electical dose. • Managing complications. • Shift to recovery room till patient concious and stable.
- 18. Muscrainic anti-cholinergic: • Administered before anesthetic agent • To minimize oral and respiratory secretions. • Atropine 0.3-0.6 mg IM or SC 30-60 minutes before anesthetic agent OR • 0.4-1.0 mg IV 2 or 3 minutes before anesthetic • Suxamethonium Chloride 0.5-1mg/kg i/v bolus
- 19. Anesthetic agent. • Methohexital (BREVITAL) ( most commonly used) • 0.75-1mg/kg iv bolus • Thiopental (PENTOTHAL) 2-3mg/kg iv bolus
- 20. Other anesthetic agents used.
- 21. Muscle relaxant. • After onset of anesthetic effect within a minute. • To minimize risk of bone fractures and other injuries. • Succinylcholine 0.5-1 mg/kg iv bolus.
- 22. Application of electrodes. • Clear skin • Moist skin ( dry electrodes can cause skin burns/excessive moisture can cause shortening & prevent seizure exposure.) • Position of electrodes • Unilateral electrode: • On non-dominant side. • 3cm above mid-point line between external angle of orbit & external auditory meatus. • Bilateral electrode: • 2nd electrode. Either of two points can be used. • i) At least 10cm away from 1st one. Vertically above meatus of same side. or • ii) Electrodes are placed on opposite sides of head.
- 24. Electical dose. • For unilateral fixed ECT: 400 milicoloumbs • For Bilateral ECT: 100-200 milicoloumbs. • Seizure threshold increased in men. • For age <40 • Starting dose: 150 milicoloumbs. • Dose might be increased if seizure was short or absent.
- 26. Signs of seizure. 1st • Muscle of face begin to twitch & mouth drops open. Then. • Upper eyelids, thumbs & big toe jerks rhythmically for 1½ minute. • Seizure duration: 20-50seconds.
- 27. Monitoring by EEG • Many modern ECT machines now include EEG monitoring, which helps to prevent unwarranted re- stimulation, as well as to detect prolonged seizures.
- 29. Concomitant medications. • Anti-depressant & anti-psychotics decrease seizure threshold. • Benzodiazepine should be withdrawn because of anti- convulsant effect. • Valproate & lamotrigine increase threshold. • Clozapine and Bupropion should be withdrawn because associated with late appearing seizures. • Cognitive impairment when ECT given with Lithium. • SSRIs prolong seizure duration. • Lidocaine should not be administred as increase seizure threshold. • Theophylline contraindicated as increases seizure duration. • Reserpine also contraindicated as compromise respiratory and CVS during ECT
- 30. Complications. • Prolonged and tardive seizure. • Duration > 180 seconds.(APA guidelines) • > 120 seconds ( Royal College’s revised guidelines) • Status epilepticus. • Give i/v diazepam 5-10mg immediately. • Failed stimulation. • If no seizure occurred Check machine. Check electrodes. Check contact with skin. • Charge can be increased by 50% & further stimulus can be given. • Additional procedure to lower seizure threshold include Hyperventilation and • administration of 500-2000 mg iv of Caffeine Sodium Benzoate 5-10 minutes before stimulus.
- 31. Unwanted effects • Brief Retrograde Amnesia: loss of memory up-to 30 minutes after ECT. • Brief disorientation. • Headache • Muscle pain esp. jaws. • Occasional damage to teeth, tongue or lips. • Small electical burns (due to poor application of electrodes) These unwanted effects are rare if good anesthetic technique used. Other rare complications occur due to co morbid physical illness.
- 32. Memory disorder after ECT Short-Term effects Long-Term effects Retrograde Amnesia Anterograde Amnesia Loss of memory for personnel and impersonal remote events. Dec ability to learn new information.
- 33. Frequency and number of treatments • Can be given Twice a week. • In general. 3 times/week given. • Course of ECT includes 6-12 treatments. • Little response until 2-3 treatments. • If no response after 6-8 treatments , course should be abandoned. • Prevention of relapse:- • In depression high relapse rate until continuation therapy with anti-depressants. • Maintenance ECT • At reduced frequency. • Fortnightly or monthly.
- 34. Thank you •Hope it was not an ELECTRIC SHOCK for YOU
Editor's Notes
- Thyroid, Adrenal, Sex glands & Hypothalamic dysfunction are common in patients in patients with disorders in mood, thought, motor act, feeding, sleep, sex, growth & maturation.
- The most prominent features of depression are failure to eat, loss of weight, inability to sleep, loss of interest in sex, inability to concentrate thoughts & difficulties in memory are distortion of functions