Chronic obstructive pulmonary disease
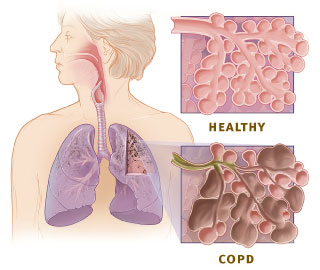
Chronic obstructive pulmonary disease (COPD) is a respiratory system disease which impedes a person from getting enough oxygen to their lungs. The lungs obtain the air a person breaths in by way of their windpipe and tubes in their lungs called bronchial tubes. These tubes, also called airways, are shaped like upside-down tree branches. At the ends of these branches are small air sacs called alveoli. The airways and sacs are made up of elastic material; this way they can change their volume to hold the appropriate amount of oxygen at any given time. The air sacs themselves act like small balloons. When you breathe in, each sac expands to contain the influx of air. Likewise, when you breathe out, the air sacs deflate as the air departs from them.
When a person has COPD, the amount of air that is transferred in and out of the airways is reduced for one of a few reasons. The reasons for this reduction could include: the airways and air sacs have lost their elastic quality, the walls between many of the air sacs have been destroyed, the walls of the airways have become thick and inflamed, or that the airways produce more mucus than normal, which clogs the airways.
COPD can be broken down into two main conditions: emphysema and chronic bronchitis. When someone has emphysema, the walls between many of the air sacs have become damaged, which causes them to become loose and floppy. This can also destroy the walls of the air sacs themselves, resulting in only a few large air sacs rather than the many necessary small ones. In contrast, chronic bronchitis causes long term swelling and a large amount of mucus in the main airways of the lungs.
COPD is a progressive disease, meaning that the person’s condition will worsen with time. COPD is a major cause of disability and stands as the fourth leading cause of death in the United States. More than twelve million people are currently diagnosed with COPD and an additional twelve million are likely to have the disease and not even know it. It is usually diagnosed in people who are middle aged or older and is not contagious. There are treatments to slow the process of COPD, but currently no doctors have been able to prevent or reverse the products of COPD. [1]
Causes
There are four proven causes for chronic obstructive pulmonary disease, the most prominent being smoking. Smoking is responsible for 90% of the cases of COPD in the United States. Not all smokers will develop COPD, but it is estimated that 15% will in their lifetime. Smoking causes many symptoms of COPD. The irritating effect of the cigarette smoke attracts cells that cause inflammation in the lungs. The smoke also stimulates the same inflammatory cells to release elastase, an enzyme that breaks down the elastic fibers in lung tissue. [2] Secondhand smoke, when inhaled in excess, can also cause COPD. [3]
It has been said that air pollution can also cause COPD. People who are subject to certain air pollutes in their work environments are more inclined to get COPD. Coal miners, construction workers, metal workers, cotton workers, etc. are exposed to pollutants such as cadmium and silica. Interstitial lung diseases are commonly associated with exposure to cadmium and silica. However, a person working in an environment where they are exposed to both these pollutants and to tobacco smoke has an even higher risk of developing COPD. A person who cooks frequently with gas powered equipment in a place where the gaseous fumes are not carefully ventilated is also prone to developing COPD. [4]
Another well proven cause for COPD is an unusual genetic disorder. The disorder, a deficiency of the protein alpha-1 antitrypsin (ATT), is responsible for less than 1% of the cases of COPD in the United States. ATT is produced by the liver, and its job is it to prevent the lung enzyme elastase from breaking down the elastic fibers (elastin) that make up the airways and alveolar walls. The manufacturing of ATT is controlled by the programming of a person’s genes. A person who has inherited two defective ATT genes, one from each parent, will either have low amounts of ATT in the blood or ATT that does not function properly. The reduction of ATT in such an individual allows the destruction of tissue in the lungs by elastase to occur unopposed. A person with this ATT deficiency could develop emphysema by an age as early as thirty or forty. [5]
Symptoms
Chronic obstructive pulmonary disease is often addressed in stages. These stages are defined by a person’s symptoms as well as a measure of how well their lungs work (lung function). FEV1 is a test result that shows how fast a person can breathe out of their lungs. It stands for Forced Expiratory Volume in one second. FEV1 is measured by machines called spirometers. The test result is expressed as a percentage of normal. For example, an FEV1 of 100% would mean that the lungs are working normally, 80% is below normal, and 30% is far below normal.
It is important to keep in mind as you read the following information that not everyone who has COPD will experience all of its symptoms; likewise, a person with these symptoms may not be experiencing COPD. If a person is experiencing the following symptoms, it is important for them to visit their doctor and possibly undergo a series of tests to reach a professional clinical diagnosis.
The stages of COPD can range from mild to very severe.
- At stage one, or mild COPD, a person begins to experience chronic coughing that often brings up mucus from the lungs. At this stage, the lung function (FEV1) is at 80% or higher.
- At stage two, or moderate COPD, a person will experience a more severe chronic cough which produces mucus. They will also begin to experience shortness of breath, especially during physical exertion. The person will also have occasional COPD flare-ups, also called exacerbations. A flare-up is defined as an instance where a person’s breathing and coughing symptoms suddenly become and remain more severe. With treatment, it is possible to recover and return to the same level of shortness of breath that the person had before the attack. These attacks are often life threatening and it is best for a person experiencing one to seek immediate medical attention. At stage two, a person’s lung function FEV1 ranges from 50% to 79%.
- Stage three, also referred to as severe COPD, is identified by a chronic cough with a continued increase of the presence of mucus. It is also identified by shortness of breath and weight loss. At this stage, a person will begin to experience more frequent and sometimes more sever COPD flare-ups. During this stage, a person is expected to have a lung function FEV of 30% to 49%.
- During stage four, also known as very severe COPD, a person experiences continued chronic coughing with a lot of mucus, shortness of breath, and weight loss. It is at this stage that a person will begin experiencing blue skin color, called cyanosis, especially in the lips, fingers, and toes. Fluid build-up will occur in the person’s legs and feet, referred to as edema. A person will also feel a fullness or tightness in their belly. They can also experience unusual fits of confusion which occurs when there is too much carbon dioxide and not enough oxygen in the blood. At this point, the person’s COPD flare-ups are extreme and very life-threatening. At stage four, a person will have a lung function FEV of 30% or lower, which may be accompanied by chronic respiratory failure, a condition where carbon dioxide remains in the lungs. [6]
Treatment
There is presently no cure for COPD; however, there are many things a person can do to relieve the symptoms and to slow the progression of the disease. [7]The goals of COPD treatment are to: prevent further deterioration in lung function, improve symptoms, and improve performance of daily activities and quality of life. There are five common treatment strategies: 1) quitting smoking if the person is a smoker, 2) taking medications to dilate airways and decrease airway inflammation, 3) vaccinating against flu influenza and pneumonia, 4) regular oxygen supplementation, and 5) pulmonary rehabilitation. [8]
The most important treatment for a smoker who has COPD is to quit smoking. Cigarette smoke itself can provoke lung deterioration and when accompanied with deterioration from something else, even as simple as ageing, it has profound effects. It is very difficult for smokers, especially longtime smokers, to quit because of their nicotine addiction. Some ideas to keep in mind when trying to quit are using nicotine gum or nicotine patches; getting into a support group, whether it be your family or a private group; and remembering that it is for the overall benefit of your health.
There are several drugs that a person can administer to lessen the effects of COPD.
Bronchodilators
- Bronchodilators are medications similar to ones used to treat bronchospasm in asthma. Their function is to relax the muscles surrounding the small airways; thereby opening them. Bronchodilators can be inhaled, taken orally, or administered intravenously. Inhaled bronchodilators are the most popular because they go directly to the airways where they are needed. Metered dose inhalers (MDIs) are used to deliver bronchodilators. A MDI is a pressurized canister which contains a medication that is released when the canister is compressed. A standard amount of medication is released each time the MDI is compressed. To maximize the delivery of the medications to the airways, the patient has to learn to inhale simultaneously with each compression. Incorrect use of the MDI can lead to deposition of much of the medication on the tongue and the back of the throat instead of in the airways. To decrease the deposition of medications on the throat and increase the amount reaching the airways, spacers can be utilized. Spacer devices can hold the released medications long enough for patients to inhale them slowly and deeply into the lungs and therefore greatly increase the proportion of medication reaching the airways.
Beta-agonists
- Beta-2 agonists are another medication administered to relieve effects of COPD. Beta-2 agonists can be administered by MDI inhalers or orally. Activation of beta-2 receptors relaxes the muscles surrounding the airways and opens the airways. Dilating airways helps relieve the symptoms of dyspnea, shortness of breath. Beta-2 agonists have been shown to relieve dyspnea in many COPD patients, even among those without possibilities of reversing airway obstruction. The action of beta-2 agonists starts within minutes after inhalation and lasts for about 4 hours. Beta-2 agonists are especially helpful for patients who suffer from severe shortness of breath because they act so quickly. This qualifies them as rescue inhalers. Because of their short duration of action, these medications are for symptoms as they develop rather than for maintenance. Evidence suggests that when these drugs are used routinely, their effectiveness is weakened. Examples of beta-2 agonists include: albuterol, metaproterenol, pirbuterol, terbutaline, isoetharine, and the newly approved Levalbuterol. Some Beta-2 agonists have a slower onset of action but a longer period of activity, such as salmeterol xinafoate, and formoterol fumarate. These drugs may be used routinely as maintenance medications. The drugs last twelve hours and should be taken a maximum of twice daily. Side effects of beta-2 agonists include anxiety; tremors; palpitations, or fast heart rate; and low blood potassium.
Anti-cholinergic Agents
- Acetylcholine is a chemical released by nerves that attaches to receptors on the muscles surrounding the airway, causing the muscles to contract and the airways to narrow. Anti-cholinergic drugs, such as ipratropium bromide, dilate airways. This is accomplished by blocking the receptors for acetylcholine on the muscles of the airways and preventing them from narrowing. Ipratropium bromide is usually administered with a MDI. In patients with COPD, ipratropium has been shown to alleviate dyspnea, improve exercise tolerance, and improve FEV1. Ipratropium has a slower onset of action but longer duration of action than the beta-2 agonists. Ipratropium is usually well-tolerated with minimal side effects even when used in high doses. Tiotropium (SPIRIVA) is a long-acting and more powerful version of Ipratropium and has been shown to be more effective than other forms. In comparing ipratropium with beta-2 agonists in the treatment of patients with COPD, studies suggest that ipratropium may be more effective in dilating airways and improving symptoms with fewer side effects. Ipratropium is especially suitable for use by elderly patients who may have difficulty with side effects of the beta-2 agonists such as fast heart rate and tremors. In patients who respond poorly to either beta-2 agonists or ipratropium alone, a combination of the two drugs sometimes results in a better response without any additional side effects.
Methylxanthines
- Theophylline and aminophylline are both examples of methylxanthines. Methylxanthines are either administered orally or intravenously. Long acting theophylline preparations can be given orally once or twice a day. Theophylline, like a beta agonist, relaxes the muscles surrounding the airways but also prevents most cells around the airways from releasing bronchoconstricting chemicals such as histamine. Theophylline also can act as a mild diuretic and increase urination. Theophylline also may increase the force of contractions of the heart and lower pressure in the pulmonary arteries. Thus, theophylline can help patients with COPD who have heart failure and pulmonary hypertension. Dosages and blood levels of theophylline or aminophylline have to be closely monitored. Excessively high levels in the blood can lead to nausea, vomiting, heart rhythm problems, and even seizures. In patients with heart failure, or cirrhosis, dosages of methylxanthines are lowered to avoid high blood levels. Interactions with other medications can also alter blood levels of methylxanthines.
Corticosteroids
- When airway inflammation contributes to airflow obstruction, anti-inflammatory medications called corticosteroids may be beneficial. Examples of corticosteroids include Prednisone and Prednisolone. Twenty to thirty percent of patients with COPD show improvement in lung function when given corticosteroids by mouth. Unfortunately, high doses of oral corticosteroids over long periods of time can have serious side effects including osteoporosis, bone fractures, diabetes mellitus, high blood pressure, thinning of the skin and easy bruising, insomnia, emotional changes, and weight gain. Therefore, many doctors use oral corticosteroids as a last resort treatment. When oral corticosteroids are used they are prescribed at the lowest possible doses for the shortest period of time to minimize side effects. When it is necessary to use long term oral steroids, accompanying medications are often prescribed to help reduce the development of possible side effects. Corticosteroids can also be inhaled. Inhaled corticosteroids have less effects than long term oral corticosteroids. Examples of inhaled corticosteroids include beclomethasone dipropionate, triamcinolone acetonide, fluticasone, budesonide, mometasone furoate and flunisolide. Inhaled corticosteroids are usually utilized for treating patients with asthma rather than the oral forms. However, it is not yet clear whether inhaled corticosteroids have the same benefit as oral corticosteroids when it comes to COPD patients. Nevertheless, doctors are less concerned about using inhaled corticosteroids because they have fewer side effects. These side effects include hoarseness, loss of voice, and oral yeast infections.
Alpha-1 antitrypsin injections
- As mentioned before, ATT deficiencies can be responsible for causing COPD. Replacement of missing or inactive ATT by injection can help prevent progression of emphysema, but has no benefit with other types of COPD. [9]
There are also other steps a person can take to relieve symptoms of COPD without utilizing drugs.
Passage Drainage Procedures
- When having difficulty with bronchial drainage, a person is recommended to try some of the following steps: sit erected to encourage draining, try controlled coughing to remove the congestion, and drink lots of fluids. [10]
Stay active
- When a person with COPD remains active, they are less likely to have shortness of breath. It will most likely also improve their outlook on life and prevent them from falling into depression.
Stay healthy
- People with COPD are more prone to illnesses, especially pneumonia and the flu. It is wise for them to wash their hands often, avoid people who are sick, and possibly get an annual flu shot. It is also important to eat healthy to keep up their immune system and overall health.
Avoid triggers
- It is best for a person with COPD to distance themselves from anything that could trigger a flare-up. Such things could include indoor and outdoor air pollution, cold dry air, hot humid air, and high altitudes.
Learn how to breathe
- It is important for people who have COPD to learn ways to breathe that improve airflow in and out of their lungs. It is also smart for them to find ways to clear their lungs to save energy and oxygen.
Rest often
- A person with COPD should not be afraid to take breaks throughout the day, such as during household chores or other activities. A physical therapist would be a wise person to consult about finding ways to do everyday activities without exerting much effort. [11]
There are also more severe measures that a person with COPD could take in attempt to slow or reverse its effects.
Home oxygen therapy
- In cases with hypoxemia (low blood oxygen) supplemental oxygen is prescribed to improve the physical and mental functioning of patients. Several studies have shown greater long-term survival in patients with severe COPD who received oxygen therapy than those who did not.
Surgery
- Lung transplants are sometimes considered for people with more severe cases of COPD. Another option is lung volume reduction surgery (LVRS). In LVRS, the surgeon removes small wedges of damaged tissue, usually 20 to 30 percent of each lung. Removing some damaged air sacs reduces the size of the lungs. As a result, the diaphragm contracts and relaxes more effectively and efficiently, improving air exchange. Results of a large clinical trial, called the National Emphysema Treatment Trial, stated that LVRS can improve the lung function of many people with emphysema. In people whose emphysema occurred mainly in the upper lobes of their lungs and whose exercise capacity was still low after they had undergone several weeks of pulmonary rehab, survival rates were longer and lung function was better compared to people with similar situations who did not have the surgery. However, for people who did not have emphysema in the upper lobes of their lungs and who had a greater exercise capacity after pulmonary rehabilitation, the surgery lowered survival rates and did not result in higher lung function. [12]
Clinical Research

A clinical study is currently underway to compare the inhalation therapy using a machine which administers medication to the lungs by intermittent positive pressure breathing (IPPB) with one that uses a machine that delivers the medicine by relying on the patient’s own breathing. Although the home use of IPPB machines is widespread, previous studies have not been able to prove if their use was effective. In this new study, nine hundred and eighty-five patients with COPD were randomly assigned to either receive a bronchodilator aerosol solution by IPPB or to receive the medication via a compressor nebulizer. The only difference between the patients who received different treatment methods was the positive pressure applied by the IPPB. There was no significant statistic difference between the methods in numbers of deaths, frequency and length of hospitalization, change in lung function tests, or in measurements of quality of life. This study suggests that the use of IPPB devices may be unnecessary. [13]
References
- Google health-COPD 2009
- What is COPD? by the National Heart, Lung, and Blood Institute. March 2009
- COPDOctober 20, 2009
- COPD articleMedicineNet Inc.,
- Overview of COPDMedscape
- Report on COPDRobert A. Wise, April 2007
- Familydoctor.org article on COPDAugust 2001
- COPD articleWebMD, 2009
- Novartis report on COPDNovartis Pharmaceuticals Corporation, 2009
- Intro to COPDHealth Grades Inc., 2009
- WebMD report on COPDWebMD 2005
- Mayo Foundation Research on COPDMayo Foundation for Medical Education and Research, 2001
- COPD treatmentHealthcomunities.com Inc., 1998
Other respiratory diseases
- Acute respiratory distress syndrome
- Asthma
- Chronic obstructive pulmonary disease
- Influenza
- Lung cancer
- Lung disease
- Measles
- Mesothelioma